Soap Acronym Social Work . They provide a clear and concise record, ensuring. Looking for software that comes equipped with social work case note templates or a soap notes example? The next acronym in the soap writing method stands for objective. Soap is an acronym for the 4 sections, or headings, that each progress note contains: Soap notes are a specific format for writing progress notes as a behavioral health clinician. This section is for the social worker, medical, or mental health. This guide provides detailed instructions for each section of. A soap note is a structured method used for documenting a patient's medical information during a therapy session. They contain four primary sections, represented by its acronym: In social work, soap notes are essential for recording client sessions, assessing progress, and strategizing future interventions. Where a client’s subjective experiences, feelings, or perspectives are recorded. Soap notes are essential for effective patient care and documentation in clinical social work. The soap acronym stands for subjective, objective, assessment, and plan, which are.
from www.template.net
Soap notes are a specific format for writing progress notes as a behavioral health clinician. Where a client’s subjective experiences, feelings, or perspectives are recorded. Soap notes are essential for effective patient care and documentation in clinical social work. They contain four primary sections, represented by its acronym: Looking for software that comes equipped with social work case note templates or a soap notes example? The soap acronym stands for subjective, objective, assessment, and plan, which are. This section is for the social worker, medical, or mental health. In social work, soap notes are essential for recording client sessions, assessing progress, and strategizing future interventions. They provide a clear and concise record, ensuring. This guide provides detailed instructions for each section of.
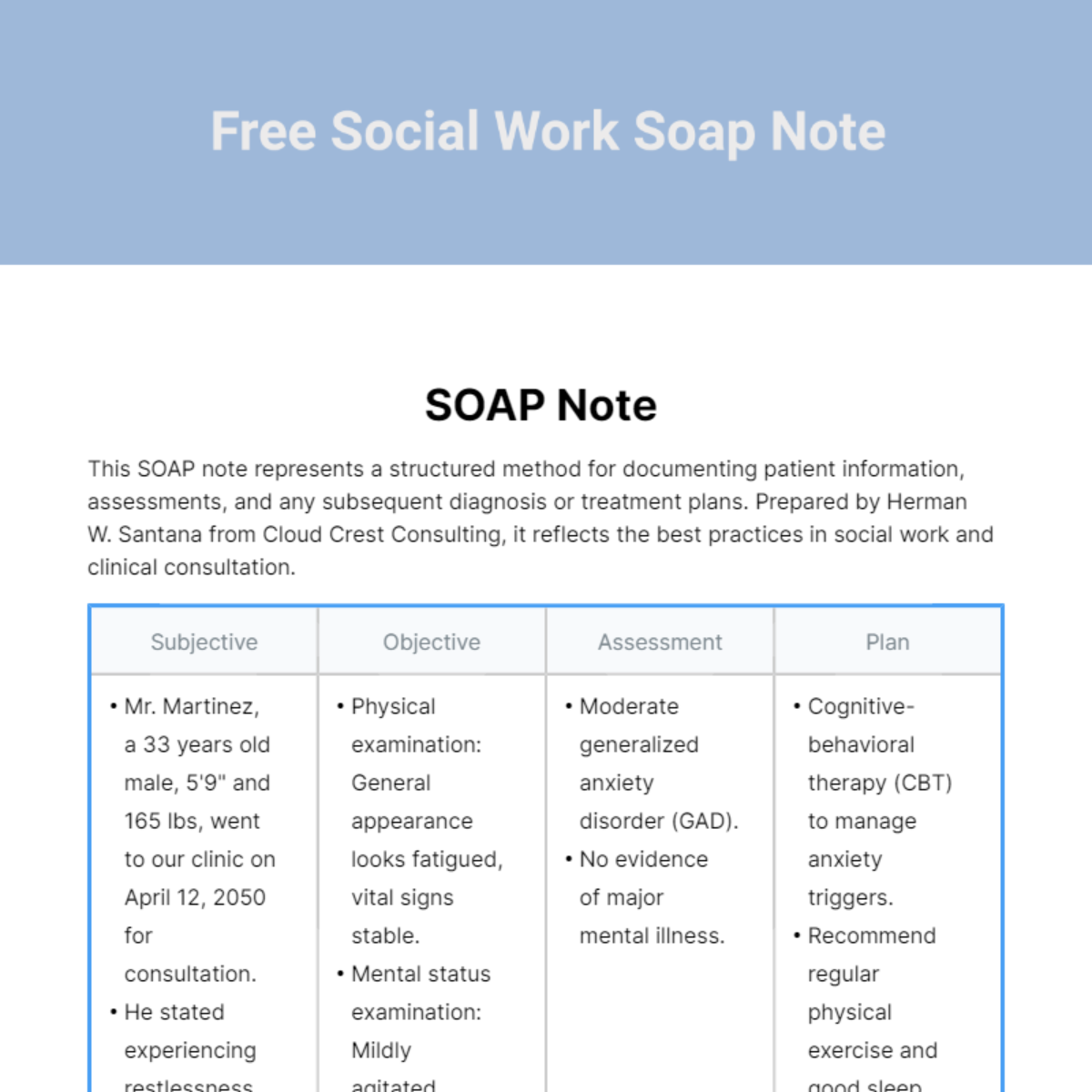
Social Work Soap Note Template Edit Online & Download Example
Soap Acronym Social Work They provide a clear and concise record, ensuring. This section is for the social worker, medical, or mental health. The soap acronym stands for subjective, objective, assessment, and plan, which are. Looking for software that comes equipped with social work case note templates or a soap notes example? A soap note is a structured method used for documenting a patient's medical information during a therapy session. This guide provides detailed instructions for each section of. Soap is an acronym for the 4 sections, or headings, that each progress note contains: The next acronym in the soap writing method stands for objective. Soap notes are a specific format for writing progress notes as a behavioral health clinician. Soap notes are essential for effective patient care and documentation in clinical social work. In social work, soap notes are essential for recording client sessions, assessing progress, and strategizing future interventions. They provide a clear and concise record, ensuring. They contain four primary sections, represented by its acronym: Where a client’s subjective experiences, feelings, or perspectives are recorded.
From www.socialworkportal.com
How to Write a Social Work Soap Assessment Best Guide to Soap Soap Acronym Social Work They contain four primary sections, represented by its acronym: The soap acronym stands for subjective, objective, assessment, and plan, which are. Soap notes are a specific format for writing progress notes as a behavioral health clinician. They provide a clear and concise record, ensuring. Soap is an acronym for the 4 sections, or headings, that each progress note contains: Soap. Soap Acronym Social Work.
From klaazngam.blob.core.windows.net
Soap Note Example Social Work at Marie Bramlett blog Soap Acronym Social Work A soap note is a structured method used for documenting a patient's medical information during a therapy session. This section is for the social worker, medical, or mental health. The next acronym in the soap writing method stands for objective. Looking for software that comes equipped with social work case note templates or a soap notes example? In social work,. Soap Acronym Social Work.
From www.pinterest.com
Tips for Writing Better Mental Health SOAP Notes Health information Soap Acronym Social Work This guide provides detailed instructions for each section of. A soap note is a structured method used for documenting a patient's medical information during a therapy session. The next acronym in the soap writing method stands for objective. They provide a clear and concise record, ensuring. Where a client’s subjective experiences, feelings, or perspectives are recorded. In social work, soap. Soap Acronym Social Work.
From klaazngam.blob.core.windows.net
Soap Note Example Social Work at Marie Bramlett blog Soap Acronym Social Work The next acronym in the soap writing method stands for objective. Where a client’s subjective experiences, feelings, or perspectives are recorded. Soap notes are a specific format for writing progress notes as a behavioral health clinician. They contain four primary sections, represented by its acronym: Soap is an acronym for the 4 sections, or headings, that each progress note contains:. Soap Acronym Social Work.
From klaazngam.blob.core.windows.net
Soap Note Example Social Work at Marie Bramlett blog Soap Acronym Social Work Where a client’s subjective experiences, feelings, or perspectives are recorded. Soap is an acronym for the 4 sections, or headings, that each progress note contains: The soap acronym stands for subjective, objective, assessment, and plan, which are. Soap notes are essential for effective patient care and documentation in clinical social work. The next acronym in the soap writing method stands. Soap Acronym Social Work.
From printablelibmario.z19.web.core.windows.net
Soap Note Template For Social Work Soap Acronym Social Work Looking for software that comes equipped with social work case note templates or a soap notes example? This guide provides detailed instructions for each section of. The next acronym in the soap writing method stands for objective. Where a client’s subjective experiences, feelings, or perspectives are recorded. A soap note is a structured method used for documenting a patient's medical. Soap Acronym Social Work.
From printablelibmario.z19.web.core.windows.net
Soap Note Template For Social Work Soap Acronym Social Work They contain four primary sections, represented by its acronym: In social work, soap notes are essential for recording client sessions, assessing progress, and strategizing future interventions. Where a client’s subjective experiences, feelings, or perspectives are recorded. They provide a clear and concise record, ensuring. This section is for the social worker, medical, or mental health. The soap acronym stands for. Soap Acronym Social Work.
From www.socialwork.career
The Two Acronyms You Must Know for the LMSW Exam SocialWork.Career Soap Acronym Social Work Soap notes are essential for effective patient care and documentation in clinical social work. Where a client’s subjective experiences, feelings, or perspectives are recorded. Soap is an acronym for the 4 sections, or headings, that each progress note contains: They provide a clear and concise record, ensuring. Looking for software that comes equipped with social work case note templates or. Soap Acronym Social Work.
From www.pinterest.com.au
The Subjective, Objective, Assessment and Plan (SOAP) note is an Soap Acronym Social Work They contain four primary sections, represented by its acronym: Soap notes are essential for effective patient care and documentation in clinical social work. A soap note is a structured method used for documenting a patient's medical information during a therapy session. Soap notes are a specific format for writing progress notes as a behavioral health clinician. This guide provides detailed. Soap Acronym Social Work.
From narodnatribuna.info
The Mesmerizing 35 Soap Note Examples Blank Formats Soap Acronym Social Work They contain four primary sections, represented by its acronym: This guide provides detailed instructions for each section of. Soap notes are a specific format for writing progress notes as a behavioral health clinician. Where a client’s subjective experiences, feelings, or perspectives are recorded. This section is for the social worker, medical, or mental health. Soap is an acronym for the. Soap Acronym Social Work.
From www.cambridge.org
List of acronyms Mental Health Social Work Reimagined Soap Acronym Social Work The next acronym in the soap writing method stands for objective. Soap is an acronym for the 4 sections, or headings, that each progress note contains: This guide provides detailed instructions for each section of. They provide a clear and concise record, ensuring. In social work, soap notes are essential for recording client sessions, assessing progress, and strategizing future interventions.. Soap Acronym Social Work.
From thinkinpossibilities.com
Social Work SOAP Notes Forms Printable Digital Download Think in Soap Acronym Social Work Soap notes are essential for effective patient care and documentation in clinical social work. They contain four primary sections, represented by its acronym: The soap acronym stands for subjective, objective, assessment, and plan, which are. This section is for the social worker, medical, or mental health. Where a client’s subjective experiences, feelings, or perspectives are recorded. Looking for software that. Soap Acronym Social Work.
From in.pinterest.com
First Aid CPD SOAP 👀⠀ ⠀ SOAP is a medical acronym used to remember Soap Acronym Social Work The soap acronym stands for subjective, objective, assessment, and plan, which are. This guide provides detailed instructions for each section of. Soap notes are essential for effective patient care and documentation in clinical social work. They contain four primary sections, represented by its acronym: Looking for software that comes equipped with social work case note templates or a soap notes. Soap Acronym Social Work.
From gioqgucws.blob.core.windows.net
Soap Acronym Mental Health at Eric Rousseau blog Soap Acronym Social Work Soap notes are essential for effective patient care and documentation in clinical social work. Where a client’s subjective experiences, feelings, or perspectives are recorded. They provide a clear and concise record, ensuring. The next acronym in the soap writing method stands for objective. They contain four primary sections, represented by its acronym: Soap notes are a specific format for writing. Soap Acronym Social Work.
From www.advantismed.com
How to Master Nurse Charting & Avoid Mistakes Soap Acronym Social Work In social work, soap notes are essential for recording client sessions, assessing progress, and strategizing future interventions. They provide a clear and concise record, ensuring. They contain four primary sections, represented by its acronym: The next acronym in the soap writing method stands for objective. Soap notes are essential for effective patient care and documentation in clinical social work. This. Soap Acronym Social Work.
From eloisewilkinson.z21.web.core.windows.net
Soap Chart Note Is An Acronym For Soap Acronym Social Work Where a client’s subjective experiences, feelings, or perspectives are recorded. Looking for software that comes equipped with social work case note templates or a soap notes example? In social work, soap notes are essential for recording client sessions, assessing progress, and strategizing future interventions. The next acronym in the soap writing method stands for objective. The soap acronym stands for. Soap Acronym Social Work.
From www.powerdiary.com
Essential Guide to SOAP Notes SOAP Notes Example Soap Acronym Social Work They contain four primary sections, represented by its acronym: The next acronym in the soap writing method stands for objective. This section is for the social worker, medical, or mental health. Soap notes are a specific format for writing progress notes as a behavioral health clinician. Looking for software that comes equipped with social work case note templates or a. Soap Acronym Social Work.
From samanthapatterson.z19.web.core.windows.net
Soap Chart Note Is An Acronym For Soap Acronym Social Work This guide provides detailed instructions for each section of. Soap is an acronym for the 4 sections, or headings, that each progress note contains: The next acronym in the soap writing method stands for objective. A soap note is a structured method used for documenting a patient's medical information during a therapy session. They contain four primary sections, represented by. Soap Acronym Social Work.
From www.socialworkportal.com
How to Write a Social Work Soap Assessment Best Guide to Soap Soap Acronym Social Work Soap is an acronym for the 4 sections, or headings, that each progress note contains: Soap notes are essential for effective patient care and documentation in clinical social work. They provide a clear and concise record, ensuring. This section is for the social worker, medical, or mental health. Looking for software that comes equipped with social work case note templates. Soap Acronym Social Work.
From www.eslprintables.com
English worksheets SOAPS Acronym Soap Acronym Social Work Looking for software that comes equipped with social work case note templates or a soap notes example? The soap acronym stands for subjective, objective, assessment, and plan, which are. This guide provides detailed instructions for each section of. Soap notes are a specific format for writing progress notes as a behavioral health clinician. Where a client’s subjective experiences, feelings, or. Soap Acronym Social Work.
From printabletemplate.concejomunicipaldechinu.gov.co
Soap Note Template Social Work Soap Acronym Social Work They contain four primary sections, represented by its acronym: Looking for software that comes equipped with social work case note templates or a soap notes example? Where a client’s subjective experiences, feelings, or perspectives are recorded. This section is for the social worker, medical, or mental health. The soap acronym stands for subjective, objective, assessment, and plan, which are. Soap. Soap Acronym Social Work.
From gioqgucws.blob.core.windows.net
Soap Acronym Mental Health at Eric Rousseau blog Soap Acronym Social Work They provide a clear and concise record, ensuring. A soap note is a structured method used for documenting a patient's medical information during a therapy session. The next acronym in the soap writing method stands for objective. This section is for the social worker, medical, or mental health. Soap is an acronym for the 4 sections, or headings, that each. Soap Acronym Social Work.
From www.youtube.com
SOAP Notes for Social Work YouTube Soap Acronym Social Work This guide provides detailed instructions for each section of. The soap acronym stands for subjective, objective, assessment, and plan, which are. Soap notes are a specific format for writing progress notes as a behavioral health clinician. Where a client’s subjective experiences, feelings, or perspectives are recorded. They contain four primary sections, represented by its acronym: A soap note is a. Soap Acronym Social Work.
From medium.com
What is a Soap Note. According to Physiopedia SOAP notes are… by Soap Acronym Social Work They provide a clear and concise record, ensuring. Soap notes are essential for effective patient care and documentation in clinical social work. A soap note is a structured method used for documenting a patient's medical information during a therapy session. The soap acronym stands for subjective, objective, assessment, and plan, which are. Soap notes are a specific format for writing. Soap Acronym Social Work.
From aliciawatts.z13.web.core.windows.net
Soap Chart Note Is An Acronym For Soap Acronym Social Work Where a client’s subjective experiences, feelings, or perspectives are recorded. The soap acronym stands for subjective, objective, assessment, and plan, which are. In social work, soap notes are essential for recording client sessions, assessing progress, and strategizing future interventions. This section is for the social worker, medical, or mental health. A soap note is a structured method used for documenting. Soap Acronym Social Work.
From klaazngam.blob.core.windows.net
Soap Note Example Social Work at Marie Bramlett blog Soap Acronym Social Work They provide a clear and concise record, ensuring. This guide provides detailed instructions for each section of. A soap note is a structured method used for documenting a patient's medical information during a therapy session. The next acronym in the soap writing method stands for objective. The soap acronym stands for subjective, objective, assessment, and plan, which are. Where a. Soap Acronym Social Work.
From klaazngam.blob.core.windows.net
Soap Note Example Social Work at Marie Bramlett blog Soap Acronym Social Work They contain four primary sections, represented by its acronym: This guide provides detailed instructions for each section of. A soap note is a structured method used for documenting a patient's medical information during a therapy session. Where a client’s subjective experiences, feelings, or perspectives are recorded. In social work, soap notes are essential for recording client sessions, assessing progress, and. Soap Acronym Social Work.
From www.pinterest.com
Soap notes Social Work Pinterest Soap Note, Soaps and Note Soap Acronym Social Work This guide provides detailed instructions for each section of. Where a client’s subjective experiences, feelings, or perspectives are recorded. A soap note is a structured method used for documenting a patient's medical information during a therapy session. They contain four primary sections, represented by its acronym: Soap notes are essential for effective patient care and documentation in clinical social work.. Soap Acronym Social Work.
From www.socialworkportal.com
How to Write a Social Work Soap Assessment Best Guide to Soap Soap Acronym Social Work In social work, soap notes are essential for recording client sessions, assessing progress, and strategizing future interventions. Soap notes are essential for effective patient care and documentation in clinical social work. Soap notes are a specific format for writing progress notes as a behavioral health clinician. Looking for software that comes equipped with social work case note templates or a. Soap Acronym Social Work.
From www.template.net
Social Work Soap Note Template Edit Online & Download Example Soap Acronym Social Work Soap is an acronym for the 4 sections, or headings, that each progress note contains: They provide a clear and concise record, ensuring. This section is for the social worker, medical, or mental health. Soap notes are essential for effective patient care and documentation in clinical social work. Looking for software that comes equipped with social work case note templates. Soap Acronym Social Work.
From www.pinterest.com
behavioral health soap note Medicina, Serviço social, Resolução de Soap Acronym Social Work A soap note is a structured method used for documenting a patient's medical information during a therapy session. This guide provides detailed instructions for each section of. In social work, soap notes are essential for recording client sessions, assessing progress, and strategizing future interventions. Where a client’s subjective experiences, feelings, or perspectives are recorded. They provide a clear and concise. Soap Acronym Social Work.
From gioqgucws.blob.core.windows.net
Soap Acronym Mental Health at Eric Rousseau blog Soap Acronym Social Work They contain four primary sections, represented by its acronym: This guide provides detailed instructions for each section of. Soap is an acronym for the 4 sections, or headings, that each progress note contains: A soap note is a structured method used for documenting a patient's medical information during a therapy session. They provide a clear and concise record, ensuring. Soap. Soap Acronym Social Work.
From www.socialworkportal.com
Best Social Work Processes with Examples & SOAP Notes All You Need Soap Acronym Social Work The soap acronym stands for subjective, objective, assessment, and plan, which are. The next acronym in the soap writing method stands for objective. Soap is an acronym for the 4 sections, or headings, that each progress note contains: Soap notes are a specific format for writing progress notes as a behavioral health clinician. This guide provides detailed instructions for each. Soap Acronym Social Work.
From education2research.com
The Importance of a Well Woman Exam Soap Note A Comprehensive Guide Soap Acronym Social Work Soap notes are essential for effective patient care and documentation in clinical social work. The next acronym in the soap writing method stands for objective. Soap is an acronym for the 4 sections, or headings, that each progress note contains: Looking for software that comes equipped with social work case note templates or a soap notes example? In social work,. Soap Acronym Social Work.
From clinicsense.com
Free SOAP Notes Template ClinicSense Soap Acronym Social Work This guide provides detailed instructions for each section of. They provide a clear and concise record, ensuring. Soap is an acronym for the 4 sections, or headings, that each progress note contains: The soap acronym stands for subjective, objective, assessment, and plan, which are. The next acronym in the soap writing method stands for objective. Soap notes are a specific. Soap Acronym Social Work.