September 14, 2024
Menopause And Urinary System Incontinence Treatment
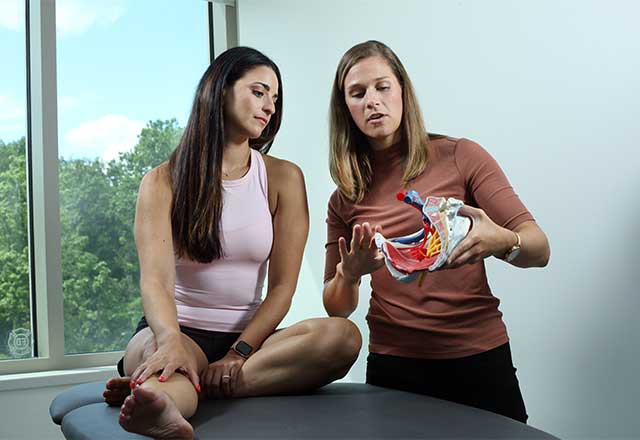
Monitoring Of Urinary Incontinence In Postmenopausal Females: An Emas Professional Overview These travel up the tibial nerve to the sacral nerve plexus, which regulates the bladder. PTNS sessions are painless, last half an hour and are repeated weekly for 12 weeks. Because of this, imipramine may work for nighttime incontinence. When used correctly, topical estrogen treatment generally doesn't create negative effects.Electric Stimulation-- A Genuine Option For Mixed Incontinence
The frequency of stress and anxiety urinary incontinence comes to a head in the 5th years and then declines, whereas the prevalence of both blended and urgency urinary incontinence remains to boost with age. Empirical information are from France, Germany, Spain and the United Kingdom180. Mean occurrence information from a review of epidemiological research studies from around the globe have revealed similar trends22. Mixed urinary incontinence is a type of urinary incontinence that happens when an individual experiences a combination of stress incontinence and prompt incontinence.Locate A Treatment Center
These distinctions in situation meanings relate to the moment duration over which symptoms are identified and whether signs and symptom regularity, severity and trouble are assessed. Without a doubt, research studies specifically measuring severe urinary system incontinence, specified as urine leak numerous times per week, have an even more constant reported prevalence of 6-- 10% in Europe and the United States26,30. For people with urinary incontinence, it is very important to seek advice from a health care service provider. In a lot of cases, patients will certainly after that be described an urogynecologist or urologist, a medical professional who specializes in diseases of the urinary system. Urinary system incontinence is diagnosed with a total physical examination that concentrates on the urinary system and nerves, reproductive organs, and urine examples. Changes in the bladder and urethra during menopause can likewise add to urinary system incontinence. The bladder muscular tissue can come to be much less flexible, resulting in a reduction in bladder ability and an increased frequency of peeing. Furthermore, the urethra can come to be shorter and much less elastic, making it more difficult to preserve continence. These anatomical adjustments can result in a heightened sensitivity to bladder filling, triggering an immediate requirement to urinate also when the bladder is not full. The loss of estrogen can likewise lead to thinning of the urethral lining, more jeopardizing its capacity to work effectively and increasing the chance of incontinence. If you are overweight, even 5% fat burning can boost urinary necessity substantially.Support Groups And Therapy
Is walking helpful for urinary incontinence?
Pick activities that will minimize pressure on your bladder, such as yoga and swimming. CHOOSE lower impact exercises, such as walking or Pilates. CHOOSE exercise devices that don't apply pressure on the hips, such as a treadmill or elliptical exerciser.
- By having a clear understanding, you will certainly be better prepared to understand treatment options and enhance your lifestyle.
- These factors deteriorate the overall performance of the body, causing weakness of the muscles or bones, respiratory system disorders and blood circulation problems.
- The testimonial located that ladies receiving regional (vaginal) oestrogen reported considerable improvement in their incontinence symptoms compared to sugar pill.
- Your physician might also recommend altering different medications that you're already taking for other points, such as high blood pressure, as they can raise pee result.
- These exercises are done by training, holding and afterwards unwinding your pelvic floor muscular tissues.
Social Links