

The typical recovery time after cervical spine surgery can vary depending on the specific procedure performed and the individual patient. In general, it may take several weeks to several months for a patient to fully recover. During the initial recovery period, patients may experience pain and discomfort, and they may need to wear a neck brace or collar to support the healing spine. Physical therapy is often recommended to help regain strength and mobility in the neck and upper body. It is important for patients to follow their surgeon's post-operative instructions and attend all follow-up appointments to ensure a successful recovery.
Like any surgical procedure, cervical spine surgery carries certain risks and potential complications. These can include infection, bleeding, damage to nerves or blood vessels, and adverse reactions to anesthesia. There is also a risk of complications specific to the cervical spine, such as spinal cord injury, spinal fluid leakage, or failure of the fusion to heal properly. It is important for patients to discuss these risks with their surgeon before undergoing the procedure and to closely follow all post-operative instructions to minimize the risk of complications.
Author: Mario Bizzini, PhD, MSc, PT I arrived in Tokyo on Thursday January 4th after a 12 hour flight from Zürich. With two Japanese long-time friends, I walked around some familiar spots such as the Asakusa district and the Skytree tower, and of course we also visited a couple of fine sushi restaurants. In the [...] Read More... The post Diary blog – “Mario in Japan” – Swiss Sports Physiotherapy Association appeared first on BJSM blog - social media's leading SEM voice.
Posted by on 2024-02-12
This blog is based on a recently published study exploring the link between walking speed and type 2 diabetes (1). Why is this study important? Type 2 diabetes is one of the most common metabolic disorders worldwide. Those with type 2 diabetes are at greater risk of many cancers, cardiovascular disease, and premature death. Currently, [...] Read More... The post Walking speed and Type 2 diabetes appeared first on BJSM blog - social media's leading SEM voice.
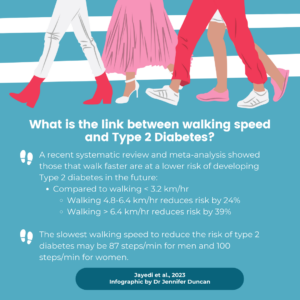
Posted by on 2024-02-09
Keywords: Knee, meniscal tear, structural damage This blog is based on a recent study exploring differences in structural knee joint damage [1]. Why is this study important? Recently, two randomized trials compared a strategy of early meniscal surgery to a strategy of exercise therapy with the option of later surgery (if needed) in young active [...] Read More... The post Concern for knee joint damage should not influence the choice of treatment strategy in young patients with meniscal tears. appeared first on BJSM blog - social media's leading SEM voice.

Posted by on 2024-02-04
The incision made during cervical spine surgery typically takes several weeks to heal. During this time, patients may experience some discomfort or itching around the incision site. It is important to keep the incision clean and dry, and to follow any specific care instructions provided by the surgeon. Patients should avoid picking at or scratching the incision, as this can increase the risk of infection. It is also important to avoid strenuous activity or heavy lifting during the initial healing period to allow the incision to heal properly.

Physical therapy and exercises play a crucial role in the rehabilitation process after cervical spine surgery. The specific exercises recommended will depend on the individual patient's condition and the type of surgery performed. However, common exercises may include gentle range of motion exercises to improve flexibility, strengthening exercises to build muscle strength in the neck and upper body, and postural exercises to promote proper alignment and reduce strain on the cervical spine. Physical therapy sessions may also include manual therapy techniques, such as massage or joint mobilization, to help reduce pain and improve mobility.
After cervical spine surgery, there may be certain restrictions or limitations on activities to ensure proper healing and minimize the risk of complications. Patients are typically advised to avoid heavy lifting, bending, or twisting of the neck for a certain period of time. They may also need to wear a neck brace or collar during the initial recovery period to provide support and stability to the healing spine. It is important for patients to follow their surgeon's instructions regarding activity restrictions and gradually increase their activity level as directed.

The time it takes for the neck muscles to regain strength after cervical spine surgery can vary depending on the individual patient and the extent of the surgery. In general, it may take several weeks to several months for the muscles to regain their full strength. Physical therapy plays a crucial role in this process, as it helps to gradually strengthen and condition the muscles through targeted exercises. It is important for patients to be consistent with their physical therapy exercises and to follow their therapist's recommendations to optimize muscle recovery and regain strength in the neck.
Signs of a potential infection after cervical spine surgery include increased pain, redness, swelling, warmth, or drainage around the incision site. If a patient experiences any of these symptoms, it is important to contact their doctor immediately. Other signs of infection may include fever, chills, or a general feeling of illness. Prompt medical attention is crucial in order to diagnose and treat any infection early to prevent further complications. Patients should closely follow their surgeon's post-operative instructions regarding wound care and hygiene to minimize the risk of infection.

Yes, there is a difference in rehab protocols for partial versus complete ACL tears. When it comes to partial ACL tears, the rehab protocols focus on conservative management and non-surgical interventions. These may include physical therapy exercises to strengthen the surrounding muscles, bracing or taping to provide stability, and activity modification to avoid further damage. On the other hand, complete ACL tears often require surgical intervention followed by a more intensive rehabilitation program. This may involve a combination of pre-operative and post-operative exercises to restore range of motion, strengthen the muscles, and improve stability. The rehab protocols for complete ACL tears also emphasize on functional training and sport-specific exercises to help individuals return to their pre-injury level of activity.
The recommended approach for rehabilitating a dislocated shoulder involves a comprehensive and individualized treatment plan that focuses on reducing pain, restoring range of motion, and strengthening the surrounding muscles. Initially, the patient may undergo a period of immobilization using a sling or brace to allow the shoulder joint to heal. Physical therapy plays a crucial role in the rehabilitation process, with exercises targeting the rotator cuff, deltoid, and scapular stabilizers. These exercises may include shoulder stretches, range of motion exercises, and progressive resistance training. Additionally, modalities such as heat or cold therapy, ultrasound, and electrical stimulation may be used to alleviate pain and promote healing. The rehabilitation program may also incorporate proprioceptive training, balance exercises, and functional activities to improve joint stability and prevent future injuries. It is important for the patient to follow the guidance of a qualified healthcare professional throughout the rehabilitation process to ensure optimal recovery and minimize the risk of reinjury.
There are indeed dietary recommendations that can support orthopedic rehab. Consuming a balanced diet rich in nutrients such as protein, calcium, vitamin D, and omega-3 fatty acids can aid in the healing and recovery of orthopedic injuries. Protein is essential for tissue repair and muscle strength, while calcium and vitamin D are crucial for bone health and density. Omega-3 fatty acids have anti-inflammatory properties that can help reduce swelling and promote healing. Additionally, maintaining a healthy weight through proper nutrition can alleviate stress on the joints and facilitate the rehabilitation process. It is important for individuals undergoing orthopedic rehab to consult with a healthcare professional or registered dietitian to develop a personalized dietary plan that meets their specific needs and supports their recovery goals.
Physical therapy plays a crucial role in the management of patellofemoral pain syndrome (PFPS) by employing a comprehensive approach that addresses the underlying causes and symptoms of the condition. Through a combination of targeted exercises, manual therapy techniques, and patient education, physical therapists aim to alleviate pain, improve joint mechanics, and enhance functional abilities. Specific exercises such as quadriceps strengthening, hip and core stabilization, and flexibility training help to rebalance muscle imbalances, improve patellar tracking, and reduce excessive stress on the patellofemoral joint. Manual therapy techniques, including soft tissue mobilization and joint mobilization, can further alleviate pain and improve joint mobility. Additionally, physical therapists educate patients on proper biomechanics, activity modification, and self-management strategies to prevent future flare-ups and promote long-term recovery. By addressing the multifactorial nature of PFPS, physical therapy plays a vital role in the successful management of this condition.
To prevent muscle atrophy during immobilization post-surgery, it is crucial to engage in specific exercises and physical therapy techniques that target the affected muscles and surrounding areas. These exercises should focus on maintaining muscle strength, flexibility, and range of motion. Additionally, incorporating resistance training, such as using weights or resistance bands, can help stimulate muscle growth and prevent muscle wasting. It is also important to follow a balanced and nutritious diet that provides adequate protein and essential nutrients to support muscle health and recovery. Regular monitoring and assessment by a healthcare professional or physical therapist can ensure that the exercise program is tailored to the individual's specific needs and progress.
Electrical stimulation plays a crucial role in orthopedic rehab by promoting muscle strength, improving range of motion, and accelerating the healing process. This therapeutic modality involves the application of electrical currents to targeted muscles or nerves, which helps to activate and strengthen weakened muscles, reduce pain and inflammation, and enhance tissue repair. By delivering controlled electrical impulses, electrical stimulation can effectively stimulate muscle contractions, increase blood flow, and promote the release of endorphins, thereby facilitating the recovery and rehabilitation of orthopedic injuries. Additionally, electrical stimulation can also be used in conjunction with other rehabilitation techniques, such as exercise therapy and manual therapy, to optimize outcomes and improve functional outcomes for patients undergoing orthopedic rehab.