

There are several different types of mobilization techniques that can be used for post-fracture rehabilitation. These techniques include passive range of motion exercises, active range of motion exercises, joint mobilizations, and soft tissue mobilizations. Passive range of motion exercises involve a therapist moving the affected limb through its full range of motion, while active range of motion exercises involve the patient actively moving the limb themselves. Joint mobilizations focus on restoring normal joint movement and can include techniques such as joint glides and traction. Soft tissue mobilizations involve techniques such as massage and stretching to improve flexibility and reduce muscle tension.
The initiation of mobilization techniques after a fracture depends on several factors, including the type and severity of the fracture, the location of the fracture, and the individual patient's healing process. In general, mobilization techniques can be initiated as soon as the fracture has stabilized and there is no risk of further damage or displacement. This typically occurs once the fracture has been immobilized with a cast or splint and the bone has started to heal. However, it is important to consult with a healthcare professional to determine the appropriate timing for mobilization techniques based on the specific circumstances of the fracture.
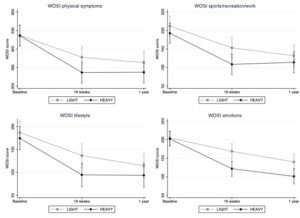
Why is this study important? Clinicians managing patients with hypermobility spectrum disorder (HSD) and shoulder symptoms constantly seek evidence-based approaches for effective interventions. This study directly addresses the comparison between high-load and low-load strengthening exercises, presenting valuable insights that can inform clinical decision-making and treatment strategies and summarises a recently published study (1). How did [...] Read More... The post Managing hypermobility spectrum disorder appeared first on BJSM blog - social media's leading SEM voice.
Posted by on 2024-02-26
Keywords Wearable technology, exercise medicine, joint arthroplasty Introduction In 2015, I wrote a BJSM Blog on “Deciding when it is time to have a knee replacement”,[1] arguing for a shift away from using structural markers to assess need for knee replacement (such as X-ray and MRI) to objective functional markers. I suggested a cut off [...] Read More... The post Using wearable technology to assist with decision-making on hip and knee replacements appeared first on BJSM blog - social media's leading SEM voice.

Posted by on 2024-02-23
Don’t lose your nerve with the ulnar nerve: A guide to working up entrapment neuropathies. Introduction: What is Ulnar Nerve Entrapment? Ulnar nerve entrapment neuropathies commonly present to MSK and orthopaedics clinics, with patient’s reporting (pins and needles, paraesthesia, or muscle weakness) that fits a typical distribution. Unpicking the site of compression of the nerve, [...] Read More... The post The MSK Playbook: Ulnar Nerve Entrapment appeared first on BJSM blog - social media's leading SEM voice.

Posted by on 2024-02-16
For fractures in weight-bearing bones, there are specific mobilization techniques that are recommended to aid in rehabilitation. These techniques focus on gradually increasing weight-bearing activities to promote bone healing and restore normal function. Weight-bearing mobilization techniques may include partial weight-bearing exercises, such as standing with support or using crutches, as well as progressive weight-bearing exercises, such as walking with assistance or using a weight-bearing device. These techniques help to stimulate bone remodeling and improve strength and stability in the affected limb.

While mobilization techniques can be beneficial for post-fracture rehabilitation, there are potential risks and complications that need to be considered. These can include pain, swelling, stiffness, and muscle weakness. There is also a risk of re-injury or further damage if mobilization techniques are not performed correctly or if the fracture has not fully healed. It is important to work with a qualified healthcare professional who can assess the individual's condition, monitor progress, and provide appropriate guidance and support to minimize the risks and complications associated with mobilization techniques.
Mobilization techniques can be used for a wide range of fractures, including complex or comminuted fractures. However, the specific techniques and timing may vary depending on the nature of the fracture and the individual patient's condition. In some cases, more conservative mobilization techniques may be initially used to protect the healing bone and surrounding tissues, while in other cases, more aggressive mobilization techniques may be necessary to restore function and prevent complications. It is important to have a thorough evaluation and individualized treatment plan to determine the most appropriate mobilization techniques for each specific fracture.

There are certain contraindications and precautions to consider when using mobilization techniques for post-fracture rehabilitation. Contraindications may include open fractures, unstable fractures, fractures with significant soft tissue damage, or fractures that require surgical intervention. Precautions may include fractures with poor bone quality, fractures in older individuals or those with underlying medical conditions, or fractures that have not fully healed. It is important to consult with a healthcare professional to assess the individual's condition and determine any contraindications or precautions that may affect the use of mobilization techniques.
The time it takes to see improvements in range of motion and functional abilities with post-fracture mobilization techniques can vary depending on several factors, including the type and severity of the fracture, the individual's healing process, and the consistency and effectiveness of the rehabilitation program. In general, improvements in range of motion and functional abilities can be seen within a few weeks to a few months of starting mobilization techniques. However, it is important to note that each individual's progress will be unique and may be influenced by various factors. Regular monitoring and reassessment by a healthcare professional can help track progress and make any necessary adjustments to the rehabilitation program.

Orthotic devices can offer both risks and benefits during rehab. On the one hand, these devices can provide support and stability to the affected area, helping to alleviate pain and prevent further injury. They can also assist in correcting biomechanical abnormalities and improving overall function. Additionally, orthotic devices can aid in the rehabilitation process by promoting proper alignment and reducing stress on the joints and muscles. However, there are also potential risks associated with their use. Improperly fitted or poorly designed orthotics can lead to discomfort, skin irritation, and even exacerbation of the underlying condition. It is crucial for healthcare professionals to carefully assess each patient's specific needs and ensure that the orthotic device is tailored to their individual requirements. Regular monitoring and adjustments may be necessary to optimize the benefits and minimize the risks of using orthotic devices during rehab.
The recommended approach for rehabilitating a Lisfranc injury in athletes involves a comprehensive and individualized treatment plan that focuses on restoring function, reducing pain, and promoting healing. The rehabilitation program typically includes a combination of physical therapy exercises, such as range of motion exercises, strengthening exercises, and proprioceptive training, to improve joint stability and mobility. Additionally, modalities such as ultrasound therapy, electrical stimulation, and cold therapy may be utilized to reduce inflammation and promote tissue healing. Athletes may also benefit from wearing orthotics or custom-made shoe inserts to provide support and stability to the affected foot. Gradual return to sport activities is recommended, with close monitoring of symptoms and progression of exercises to prevent re-injury. Overall, a multidisciplinary approach involving orthopedic surgeons, physical therapists, and athletic trainers is crucial in ensuring a successful rehabilitation outcome for athletes with Lisfranc injuries.
Orthopedic rehab can be highly beneficial in the process of regaining strength and mobility after a spinal cord injury. This specialized form of rehabilitation focuses on the musculoskeletal system, which includes the bones, joints, muscles, ligaments, and tendons. By utilizing various therapeutic techniques, such as exercises, stretches, manual therapy, and assistive devices, orthopedic rehab aims to improve the overall function and mobility of the affected individual. Additionally, it helps in reducing pain, increasing range of motion, and enhancing muscle strength. The comprehensive approach of orthopedic rehab addresses not only the physical aspects but also considers the psychological and emotional well-being of the patient. Through a combination of targeted exercises, adaptive equipment, and assistive technology, orthopedic rehab plays a crucial role in facilitating the recovery and rehabilitation process for individuals with spinal cord injuries.
One of the most effective strategies for reducing inflammation in joints during rehab is to incorporate a combination of rest, ice, compression, and elevation (RICE) therapy. This involves resting the affected joint to minimize further stress and strain, applying ice packs to the area to reduce swelling and pain, using compression bandages or braces to provide support and stability, and elevating the joint above the heart level to promote fluid drainage and reduce swelling. Additionally, nonsteroidal anti-inflammatory drugs (NSAIDs) can be used to alleviate pain and inflammation. Physical therapy exercises and stretches that focus on improving joint mobility, strength, and stability can also help reduce inflammation and promote healing. It is important to follow a well-rounded rehabilitation program that includes proper nutrition, adequate hydration, and sufficient rest to optimize the body's natural healing processes and minimize inflammation in the joints.
Orthopedic rehab is a specialized form of rehabilitation that focuses on addressing muscle tightness and stiffness. This type of rehab utilizes various techniques and interventions to alleviate these symptoms and improve overall muscle function. One common approach is through the use of manual therapy, which involves hands-on techniques such as massage, stretching, and joint mobilization to release tension and increase flexibility. Additionally, orthopedic rehab may incorporate therapeutic exercises that target specific muscle groups to strengthen and lengthen tight muscles. These exercises may include stretching, resistance training, and functional movements to improve range of motion and reduce stiffness. Other modalities such as heat therapy, cold therapy, and electrical stimulation may also be used to further relax muscles and reduce tightness. Overall, orthopedic rehab aims to address muscle tightness and stiffness through a comprehensive and individualized treatment plan that targets the underlying causes and promotes optimal muscle function.
Rehabilitation protocols for a torn labrum in the shoulder typically involve a comprehensive and individualized approach to address the specific needs of the patient. The treatment plan may include a combination of physical therapy, exercises, and modalities aimed at reducing pain, improving range of motion, and restoring strength and stability to the shoulder joint. The rehabilitation program may incorporate exercises targeting the rotator cuff muscles, scapular stabilizers, and surrounding musculature to enhance shoulder function and promote proper biomechanics. Additionally, manual therapy techniques, such as joint mobilizations and soft tissue mobilizations, may be utilized to address any associated muscle imbalances or restrictions. The rehabilitation process may also involve gradual progression of activities, including functional and sport-specific exercises, to ensure a safe return to normal activities and prevent re-injury. Close monitoring and regular reassessment by a qualified healthcare professional are crucial to ensure optimal outcomes and a successful rehabilitation journey.
Orthopedic rehab can be highly beneficial in alleviating chronic pain caused by arthritis. By focusing on the musculoskeletal system, orthopedic rehab aims to improve joint function, reduce inflammation, and enhance overall mobility. Through a combination of targeted exercises, manual therapy techniques, and specialized equipment, orthopedic rehab can help individuals with arthritis manage their pain and improve their quality of life. Additionally, orthopedic rehab may include modalities such as heat or cold therapy, electrical stimulation, and ultrasound, which can further aid in pain reduction. The comprehensive approach of orthopedic rehab addresses not only the symptoms of arthritis but also the underlying causes, making it an effective treatment option for chronic pain associated with this condition.