

Common postoperative complications after spinal fusion surgery can include infection, blood clots, nerve damage, and failure of the fusion to heal properly. Infection can occur at the surgical site and may present with symptoms such as increased pain, redness, swelling, or drainage. Blood clots can form in the legs and travel to the lungs, causing shortness of breath, chest pain, or coughing up blood. Nerve damage can result in weakness, numbness, or tingling in the arms or legs. Failure of the fusion to heal, known as pseudarthrosis, can lead to ongoing pain and may require additional surgery to correct.
The recovery time after spinal fusion surgery can vary depending on the individual and the extent of the surgery. In general, it may take several weeks to months to fully recover. During the initial postoperative period, patients may need to stay in the hospital for a few days for monitoring and pain management. After discharge, they will typically need to wear a brace or corset to support the spine and limit movement. Physical therapy may also be recommended to help regain strength and mobility. It is important to follow the surgeon's instructions and attend all follow-up appointments to ensure a successful recovery.
Below is a blog response to the BJSM blog titled “Is it scientifically valid, sensible, or safe to use biomarkers to diagnose concussion?” published on November 27th (click here to view the original blog post). A reply from the original blog authors is also included. Response: Dear Editor, We read with interest the BJSM blog post [...] Read More... The post Response to blog: “Is it scientifically valid, sensible, or safe to use biomarkers to diagnose concussion?” appeared first on BJSM blog - social media's leading SEM voice.
Posted by on 2024-01-26
Author: David Propst, PA-C In this blog post, we will discuss the importance and underutilization of the SARC-F screening tool for sarcopenia, especially in primary care settings. We will also delve into the significance of resistance exercise training and nutritional interventions in managing this condition effectively. What is Sarcopenia? Sarcopenia is a muscle disorder involving [...] Read More... The post Sarcopenia and the SARC-F: Is it the Most Important Screening That You Aren’t Doing? appeared first on BJSM blog - social media's leading SEM voice.
Posted by on 2024-01-22
Authors: Margie H Davenport, Lauren Ray, Autumn Nesdoly, Jane S Thornton, Rshmi Khurana, Tara-Leigh McHugh. The recent outstanding performances of numerous trailblazing athlete-mothers are challenging societal notions of who can successfully compete as an elite athlete. Bobsledder Elana Meyers Taylor, biathlete Anaïs Chevalier-Bouchet and luger Natalie Geisenberger all medalled at the 2022 Beijing Olympics. Within the [...] Read More... The post Coach and healthcare provider experiences working with pregnant and postpartum elite athletes appeared first on BJSM blog - social media's leading SEM voice.

Posted by on 2024-01-19
During the postoperative period after spinal fusion surgery, it is important to avoid activities that could put strain on the spine and potentially disrupt the healing process. This may include heavy lifting, bending, twisting, or participating in high-impact activities such as running or jumping. Patients should also avoid sitting or standing for prolonged periods of time and should take frequent breaks to move around and stretch. It is important to follow the surgeon's specific instructions regarding activity restrictions and gradually increase activity levels as advised.

Pain and discomfort are common after spinal fusion surgery, but there are several strategies to manage them. The surgeon may prescribe pain medication to help control pain during the initial recovery period. It is important to take the medication as directed and report any concerns or side effects to the healthcare provider. Applying ice packs to the surgical site can help reduce swelling and provide temporary pain relief. Physical therapy exercises and stretches can also help alleviate discomfort and improve mobility. It is important to communicate with the healthcare team about any pain or discomfort experienced to ensure appropriate management.
There are generally no specific dietary restrictions after spinal fusion surgery, but it is important to maintain a healthy and balanced diet to support the healing process. Eating a diet rich in fruits, vegetables, lean proteins, and whole grains can provide the necessary nutrients for tissue repair and overall health. Staying hydrated is also important for proper healing. It is advisable to avoid excessive alcohol consumption and to limit caffeine intake, as these substances can interfere with the healing process and potentially interact with pain medications.

The timing for resuming driving after spinal fusion surgery can vary depending on the individual and the specific recommendations of the surgeon. In general, patients should not drive while taking prescription pain medication, as it can impair judgment and reaction time. It is important to follow the surgeon's instructions regarding driving restrictions and to wait until pain is well-controlled and mobility is sufficient to safely operate a vehicle. It may be necessary to arrange for alternative transportation during the initial recovery period.
Signs of infection to watch out for after spinal fusion surgery include increased pain, redness, swelling, warmth, or drainage at the surgical site. Fever, chills, and fatigue can also be indicators of an infection. It is important to monitor the surgical site closely and report any concerning symptoms to the healthcare provider. Prompt treatment with antibiotics may be necessary to prevent the spread of infection. Regular follow-up appointments with the surgeon are important to monitor for signs of infection and ensure proper healing.

Orthopedic rehab can be highly beneficial in aiding the recovery process following spinal fusion surgery. This specialized form of rehabilitation focuses on restoring function and mobility to the musculoskeletal system, particularly the spine. Through a combination of targeted exercises, manual therapy techniques, and other modalities, orthopedic rehab aims to improve strength, flexibility, and overall physical well-being. By addressing specific post-surgical challenges such as pain management, scar tissue formation, and muscle imbalances, orthopedic rehab can help patients regain their independence and quality of life. Additionally, the expertise of orthopedic rehab professionals ensures that the recovery process is tailored to the individual's unique needs, promoting optimal outcomes and long-term success.
Orthopedic rehab can be an effective treatment option for alleviating symptoms of IT band syndrome. IT band syndrome, also known as iliotibial band syndrome, is a common overuse injury that affects the outer side of the knee. It is characterized by pain and inflammation along the IT band, a thick band of connective tissue that runs from the hip to the knee. Orthopedic rehab focuses on addressing the underlying causes of IT band syndrome, such as muscle imbalances, poor biomechanics, and overuse. Through a combination of targeted exercises, manual therapy, and other modalities, orthopedic rehab aims to reduce pain, improve flexibility and strength, and restore normal function. By addressing the root causes of IT band syndrome, orthopedic rehab can help individuals find relief from their symptoms and prevent future recurrences.
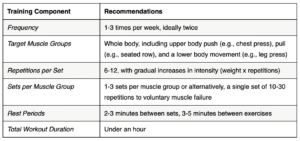
Resistance training plays a crucial role in orthopedic rehabilitation by promoting muscle strength, improving joint stability, enhancing functional capacity, and facilitating the overall recovery process. By engaging in resistance exercises, individuals undergoing orthopedic rehab can target specific muscle groups and increase their muscle mass, which in turn helps to support and protect the affected joints. Additionally, resistance training helps to improve joint stability by enhancing the coordination and control of surrounding muscles, reducing the risk of further injury or re-injury. This form of exercise also aids in restoring functional capacity by improving range of motion, flexibility, and overall physical performance. Moreover, resistance training can contribute to the management of pain and inflammation, as it stimulates the release of endorphins and promotes blood flow to the injured area. Overall, incorporating resistance training into orthopedic rehab programs can significantly enhance the recovery process and improve the long-term outcomes for individuals with orthopedic conditions.
The recommended approach for rehabilitating a Lisfranc injury involves a comprehensive and individualized treatment plan that focuses on reducing pain, restoring joint stability, improving range of motion, and promoting functional recovery. The rehabilitation program typically includes a combination of non-weight-bearing exercises, such as range of motion exercises and gentle stretching, to maintain joint mobility and prevent stiffness. Weight-bearing exercises, such as balance and proprioception training, are gradually introduced to improve stability and promote proper foot mechanics. Additionally, strengthening exercises targeting the intrinsic and extrinsic foot muscles are incorporated to enhance foot and ankle stability. Modalities such as ice, heat, ultrasound, and electrical stimulation may be used to manage pain and inflammation. The rehabilitation process also involves education on proper footwear, orthotics, and activity modification to prevent re-injury and promote long-term foot health. Close monitoring and regular follow-up with a healthcare professional are essential to ensure progress and make any necessary adjustments to the rehabilitation program.
Hydrotherapy plays a crucial role in orthopedic rehabilitation by providing a safe and effective environment for patients to regain strength, mobility, and function. The use of water as a medium for exercise and therapy allows for low-impact movements that reduce stress on joints and muscles, making it particularly beneficial for individuals recovering from orthopedic injuries or surgeries. Hydrotherapy sessions often involve a combination of exercises, such as stretching, resistance training, and cardiovascular activities, which help improve range of motion, muscle strength, and cardiovascular fitness. Additionally, the buoyancy of water provides support and reduces the effects of gravity, allowing patients to perform movements that may be challenging on land. The warm temperature of the water also helps to relax muscles, relieve pain, and promote circulation, further enhancing the rehabilitation process. Overall, hydrotherapy serves as a valuable adjunct to orthopedic rehab, facilitating faster recovery and improved outcomes for patients.