

When it comes to lumbar disc herniation, there are several effective exercises that can help alleviate symptoms and promote healing. One of the most recommended exercises is the McKenzie method, which involves a series of movements and stretches that target the lower back. These exercises aim to centralize the pain and reduce pressure on the affected disc. Other effective exercises include pelvic tilts, cat-camel stretches, and hamstring stretches. These exercises help strengthen the core muscles, improve flexibility, and promote proper alignment of the spine, which can ultimately relieve the symptoms of lumbar disc herniation.
The frequency of performing exercises for lumbar disc herniation depends on the individual's condition and the advice of their healthcare provider. In general, it is recommended to start with a few repetitions of each exercise and gradually increase the frequency and intensity over time. It is important to listen to your body and not overexert yourself. Consistency is key, so it is advisable to perform these exercises at least a few times a week to see significant improvements in symptoms and overall spinal health.
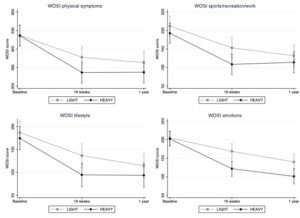
Why is this study important? Clinicians managing patients with hypermobility spectrum disorder (HSD) and shoulder symptoms constantly seek evidence-based approaches for effective interventions. This study directly addresses the comparison between high-load and low-load strengthening exercises, presenting valuable insights that can inform clinical decision-making and treatment strategies and summarises a recently published study (1). How did [...] Read More... The post Managing hypermobility spectrum disorder appeared first on BJSM blog - social media's leading SEM voice.
Posted by on 2024-02-26
Keywords Wearable technology, exercise medicine, joint arthroplasty Introduction In 2015, I wrote a BJSM Blog on “Deciding when it is time to have a knee replacement”,[1] arguing for a shift away from using structural markers to assess need for knee replacement (such as X-ray and MRI) to objective functional markers. I suggested a cut off [...] Read More... The post Using wearable technology to assist with decision-making on hip and knee replacements appeared first on BJSM blog - social media's leading SEM voice.

Posted by on 2024-02-23
Don’t lose your nerve with the ulnar nerve: A guide to working up entrapment neuropathies. Introduction: What is Ulnar Nerve Entrapment? Ulnar nerve entrapment neuropathies commonly present to MSK and orthopaedics clinics, with patient’s reporting (pins and needles, paraesthesia, or muscle weakness) that fits a typical distribution. Unpicking the site of compression of the nerve, [...] Read More... The post The MSK Playbook: Ulnar Nerve Entrapment appeared first on BJSM blog - social media's leading SEM voice.

Posted by on 2024-02-16
Author: Mario Bizzini, PhD, MSc, PT I arrived in Tokyo on Thursday January 4th after a 12 hour flight from Zürich. With two Japanese long-time friends, I walked around some familiar spots such as the Asakusa district and the Skytree tower, and of course we also visited a couple of fine sushi restaurants. In the [...] Read More... The post Diary blog – “Mario in Japan” – Swiss Sports Physiotherapy Association appeared first on BJSM blog - social media's leading SEM voice.
Posted by on 2024-02-12
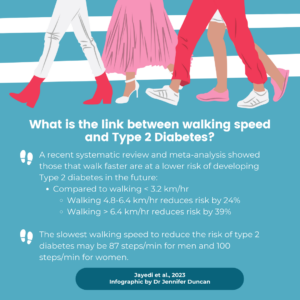
This blog is based on a recently published study exploring the link between walking speed and type 2 diabetes (1). Why is this study important? Type 2 diabetes is one of the most common metabolic disorders worldwide. Those with type 2 diabetes are at greater risk of many cancers, cardiovascular disease, and premature death. Currently, [...] Read More... The post Walking speed and Type 2 diabetes appeared first on BJSM blog - social media's leading SEM voice.
Posted by on 2024-02-09
While exercises can be beneficial for lumbar disc herniation, there are certain exercises that should be avoided to prevent further injury or aggravation of symptoms. Exercises that involve heavy lifting, twisting or bending at the waist, or high-impact activities should be avoided. These activities can put excessive strain on the lower back and potentially worsen the condition. It is important to consult with a healthcare professional or a physical therapist to determine which exercises are safe and appropriate for your specific condition.

While exercises alone may not completely cure lumbar disc herniation, they can certainly help in relieving the symptoms and promoting healing. Regular exercise can strengthen the muscles surrounding the spine, improve flexibility, and promote proper alignment of the spine. This can help reduce pressure on the affected disc and alleviate pain. However, it is important to note that exercises should be combined with other treatment modalities, such as medication, physical therapy, and lifestyle modifications, for optimal results.
When performing exercises for lumbar disc herniation, it is important to take certain precautions to prevent further injury or exacerbation of symptoms. It is advisable to start with gentle exercises and gradually increase the intensity and duration over time. It is important to maintain proper form and technique during exercises to avoid putting unnecessary strain on the lower back. It is also recommended to warm up before exercising and to stretch afterwards to prevent muscle stiffness and soreness. If any exercise causes sharp or increased pain, it should be stopped immediately, and a healthcare professional should be consulted.

While exercises can be beneficial for lumbar disc herniation, it is possible for certain exercises to worsen the condition if not performed correctly or if they put excessive strain on the lower back. It is important to listen to your body and not push through pain. If any exercise causes increased pain or discomfort, it should be avoided or modified. It is advisable to consult with a healthcare professional or a physical therapist to ensure that the exercises being performed are safe and appropriate for your specific condition.
In addition to exercises, there are alternative treatments and therapies that can be combined to enhance the effectiveness of the treatment for lumbar disc herniation. These may include chiropractic adjustments, acupuncture, massage therapy, and spinal decompression therapy. These treatments can help alleviate pain, reduce inflammation, and promote healing. It is important to consult with a healthcare professional to determine which combination of treatments and therapies would be most beneficial for your specific condition.

Physical therapy can play a crucial role in the management of osteoporosis by employing a range of specialized techniques and exercises that target the specific needs of individuals with this condition. Through the use of weight-bearing exercises, such as walking or resistance training, physical therapy can help improve bone density and strength, reducing the risk of fractures. Additionally, therapists may utilize balance and coordination exercises to enhance stability and prevent falls, which can be particularly detrimental for individuals with osteoporosis. Furthermore, manual therapy techniques, such as joint mobilization and soft tissue mobilization, can help alleviate pain and improve overall function. By tailoring treatment plans to the unique needs of each patient, physical therapy can effectively contribute to the management of osteoporosis and enhance the quality of life for individuals living with this condition.
Neuromuscular re-education plays a crucial role in orthopedic rehab by focusing on the restoration of proper movement patterns and coordination between the nervous system and muscles. It involves a variety of techniques and exercises aimed at improving proprioception, balance, and muscle control. By targeting specific muscles and their corresponding neural pathways, neuromuscular re-education helps individuals regain strength, stability, and functional movement after orthopedic injuries or surgeries. This process often includes exercises that challenge the body's ability to maintain proper alignment and control during dynamic movements, facilitating the retraining of the neuromuscular system. Additionally, neuromuscular re-education may involve the use of biofeedback devices or manual techniques to enhance sensory input and promote optimal motor responses. Overall, this approach is essential in optimizing the recovery process and preventing future injuries by re-establishing efficient neuromuscular function.
Ultrasound therapy plays a crucial role in orthopedic rehab by utilizing high-frequency sound waves to promote healing and alleviate pain in musculoskeletal conditions. This non-invasive treatment modality is commonly used in the management of various orthopedic injuries, such as fractures, sprains, strains, and tendonitis. Ultrasound therapy works by delivering deep heat to the affected area, which increases blood flow, relaxes muscles, and reduces inflammation. Additionally, it can enhance the effectiveness of other rehabilitation techniques, such as exercises and manual therapy. The use of ultrasound therapy in orthopedic rehab can expedite the recovery process, improve range of motion, and ultimately restore optimal function to the injured area.
Yes, there are several specialized physical therapy techniques that can be used to address rotator cuff injuries. One such technique is called manual therapy, which involves hands-on techniques to mobilize and manipulate the shoulder joint and surrounding tissues. This can help improve range of motion, reduce pain, and promote healing. Another technique is therapeutic exercise, which focuses on strengthening the muscles of the rotator cuff and improving overall shoulder stability. This may include exercises such as external and internal rotation, scapular stabilization exercises, and shoulder strengthening exercises. Additionally, modalities such as ultrasound, electrical stimulation, and cold therapy may be used to reduce inflammation and promote tissue healing. It is important for a physical therapist to assess the specific needs of each individual with a rotator cuff injury and tailor the treatment plan accordingly.
Stretching plays a crucial role in preventing muscle strains during rehab. When an individual undergoes rehabilitation for a muscle injury, their muscles may become tight and shortened due to immobility or disuse. Stretching exercises help to restore flexibility and lengthen the muscles, reducing the risk of strains. By elongating the muscle fibers, stretching increases the range of motion and improves muscle elasticity. This allows the muscles to withstand greater stress and reduces the likelihood of overstretching or tearing during physical activity. Additionally, stretching promotes blood flow to the muscles, delivering essential nutrients and oxygen, which aids in the healing process. It also helps to alleviate muscle imbalances and corrects any postural issues that may contribute to strain. Therefore, incorporating stretching into a rehabilitation program is essential for preventing muscle strains and promoting a successful recovery.
Manual therapy plays a crucial role in facilitating the recovery of frozen shoulder. This therapeutic approach involves hands-on techniques performed by a skilled therapist to alleviate pain, improve range of motion, and restore function in the affected shoulder joint. The therapist may employ various manual techniques such as joint mobilizations, soft tissue mobilizations, and stretching exercises to target the specific structures involved in frozen shoulder, including the joint capsule, ligaments, muscles, and tendons. By applying controlled pressure and movement to these structures, manual therapy helps to break up adhesions, release tightness, and improve the overall mobility of the shoulder joint. Additionally, manual therapy stimulates blood flow to the affected area, promoting tissue healing and reducing inflammation. This comprehensive approach not only addresses the symptoms of frozen shoulder but also addresses the underlying causes, leading to a more effective and efficient recovery process.