

High-frequency ultrasound works in medical imaging by emitting sound waves at a frequency higher than 20 MHz. These sound waves are generated by a transducer and penetrate the body's tissues. As the sound waves encounter different tissues, they are reflected back to the transducer, which then converts the echoes into electrical signals. These signals are processed by a computer to create real-time images of the internal structures of the body. High-frequency ultrasound is particularly useful in imaging superficial structures, such as the skin, as it provides detailed resolution and allows for the visualization of fine structures and abnormalities.
There are several advantages of using high-frequency ultrasound over other imaging techniques. Firstly, high-frequency ultrasound is non-invasive, meaning it does not require any incisions or injections. This makes it a safe and comfortable imaging modality for patients. Additionally, high-frequency ultrasound provides real-time imaging, allowing for immediate visualization of structures and abnormalities. It also has excellent resolution, enabling the detection of small lesions or changes in tissue morphology. Furthermore, high-frequency ultrasound is relatively inexpensive compared to other imaging techniques, making it more accessible in medical settings.
Over the last couple of years, we’ve brought you several courses focusing on Ultrasound Guided Injection Techniques. They’ve been extremely popular, and like our other courses, the feedback has been fantastic. One thing we’ve learnt along the way is that to get the most out of learning injection techniques, a solid grounding in MSK Ultrasound ...
Posted by on 2024-02-10
What a year 2023 was! We’ve loved bringing you courses covering US of the upper and lower limb, and US guided injections through the year. The mix of health professionals from all sorts of backgrounds (Doctors, Nurses, Physios, Sonographers to name a few) has been amazing to be part of. We’ve been humbled by your ...
Posted by on 2023-09-17
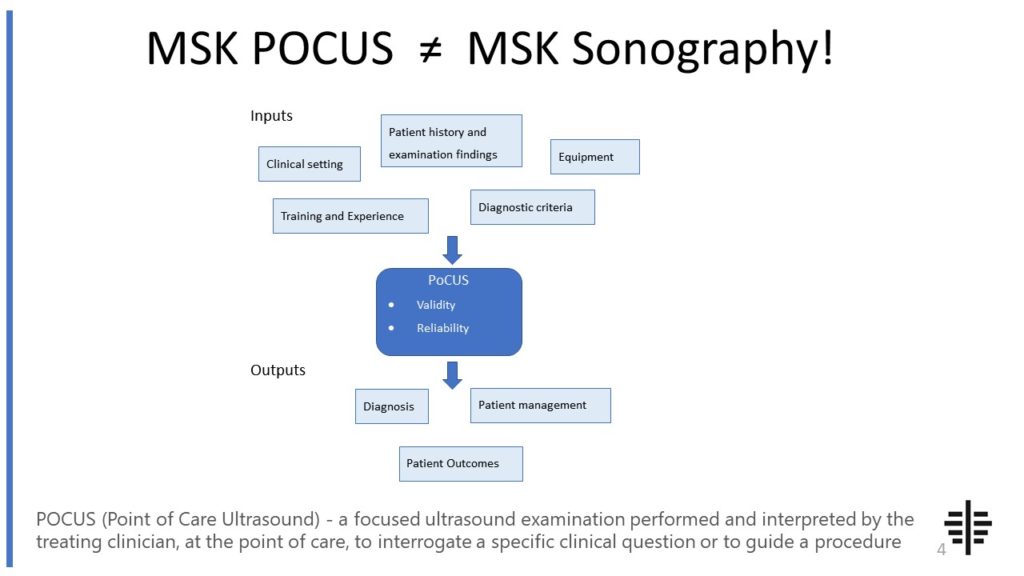
The POCUS process is very different to traditional US based in a radiology establishment. And POCUS practitioners need to be aware of those factors, unique to their particular situation, that influence diagnostic accuracy. That was the topic I presented at the plenary session of the NZAMM Annual Scientific Meeting in Wellington. A picture says 1000 ...
Posted by on 2022-10-04
We’re proud to announce that the New Zealand College of Musculoskeletal Medicine has endorsed our POCUS courses for CME and as part of vocational training. The NZCMM is responsible for setting the high standards and training of Specialist Musculoskeletal Medicine Physicians in New Zealand. NZCMM endorsement is an acknowledgement that our courses meet these standards. ...

Posted by on 2022-06-23
The RNZCUC has endorsed our courses as approved CME. We’re proud to be able to meet the training needs of Urgent Care Physicians, and look forward to meeting you at future courses.

Posted by on 2021-05-30
High-frequency ultrasound has various potential applications in dermatology. It can be used to assess skin thickness, measure the depth of skin lesions, and evaluate the extent of burns or wounds. High-frequency ultrasound can also aid in the diagnosis and monitoring of skin conditions such as acne, psoriasis, and eczema. Furthermore, it can assist in the evaluation of skin tumors, including melanoma and basal cell carcinoma. By providing detailed images of the skin and its underlying structures, high-frequency ultrasound can help dermatologists make accurate diagnoses and develop appropriate treatment plans.

High-frequency ultrasound plays a crucial role in the diagnosis and monitoring of skin cancer. It allows dermatologists to visualize the depth and extent of skin tumors, aiding in the determination of the tumor stage. High-frequency ultrasound can also help differentiate between benign and malignant lesions by assessing their characteristics, such as vascularity and tissue architecture. Additionally, it can guide the biopsy process by identifying the most appropriate area for sampling. Furthermore, high-frequency ultrasound can be used to monitor the response to treatment and detect any recurrence of skin cancer. Overall, high-frequency ultrasound enhances the accuracy and effectiveness of skin cancer diagnosis and management.
Despite its many advantages, high-frequency ultrasound has limitations in imaging deep tissues. The higher the frequency of the ultrasound waves, the more they are absorbed and scattered by tissues. This limits the penetration depth of high-frequency ultrasound, making it less effective in visualizing structures located deep within the body. Additionally, high-frequency ultrasound may have difficulty imaging structures behind bone or air-filled cavities. In these cases, other imaging modalities such as computed tomography (CT) or magnetic resonance imaging (MRI) may be more suitable for obtaining detailed images of deep tissues.

Yes, high-frequency ultrasound can be used for non-invasive monitoring of blood flow in small vessels. By using a technique called Doppler ultrasound, high-frequency ultrasound can assess the direction and velocity of blood flow in real-time. This is particularly useful in evaluating blood flow in small vessels, such as those in the skin or superficial muscles. High-frequency ultrasound can help identify abnormalities in blood flow, such as blockages or narrowing of vessels, and assist in the diagnosis of conditions such as peripheral artery disease or deep vein thrombosis. It provides a safe and efficient method for assessing blood flow without the need for invasive procedures.
High-frequency ultrasound assists in the evaluation of musculoskeletal injuries by providing detailed images of the soft tissues, muscles, tendons, and ligaments. It can help identify the extent and location of injuries, such as sprains, strains, or tears. High-frequency ultrasound can also assess the healing process of these injuries over time, allowing for appropriate treatment planning and monitoring. Additionally, it can aid in the guidance of therapeutic injections, such as corticosteroid injections for pain management. By providing real-time imaging and excellent resolution, high-frequency ultrasound is a valuable tool in the evaluation and management of musculoskeletal injuries.

Frozen shoulder syndrome, also known as adhesive capsulitis, is a condition characterized by pain and stiffness in the shoulder joint. While ultrasound is not the primary diagnostic tool for frozen shoulder syndrome, it can provide valuable information about the underlying pathology. Typical ultrasound findings in patients with frozen shoulder syndrome include thickening and inflammation of the joint capsule, as well as the presence of adhesions and fibrosis within the capsule. Additionally, ultrasound may reveal a decrease in the volume of the synovial fluid and the presence of joint effusion. These findings are indicative of the inflammatory process and the development of scar tissue within the shoulder joint, contributing to the restricted range of motion and pain experienced by patients with frozen shoulder syndrome.
Musculoskeletal ultrasound plays a crucial role in diagnosing carpal tunnel syndrome by providing detailed imaging of the musculoskeletal structures in the wrist and hand. This non-invasive imaging technique allows healthcare professionals to visualize the median nerve, tendons, ligaments, and surrounding tissues in real-time. By assessing the size and shape of the median nerve, as well as any abnormalities such as swelling or compression, musculoskeletal ultrasound can help confirm the presence of carpal tunnel syndrome. Additionally, this imaging modality can also identify other potential causes of symptoms, such as tendonitis or ganglion cysts, ensuring an accurate diagnosis and appropriate treatment plan.
Musculoskeletal ultrasound has several limitations when it comes to assessing spinal cord compression. Firstly, the technique is highly operator-dependent, meaning that the accuracy of the results can vary depending on the skill and experience of the person performing the ultrasound. Additionally, musculoskeletal ultrasound is limited in its ability to visualize structures deep within the body, such as the spinal cord. This can make it challenging to accurately assess the extent and severity of spinal cord compression. Furthermore, musculoskeletal ultrasound may not be able to provide a comprehensive evaluation of the surrounding soft tissues and bony structures, which are important in determining the underlying cause of the compression. Therefore, while musculoskeletal ultrasound can be a useful tool in the initial assessment of spinal cord compression, it should be complemented with other imaging modalities, such as magnetic resonance imaging (MRI), for a more comprehensive evaluation.
Typical ultrasound findings in patients with patellar tendinopathy include thickening and irregularity of the patellar tendon, hypoechoic areas within the tendon indicating degeneration, neovascularization, and increased vascularity. The tendon may also appear hypoechoic or hyperechoic compared to the surrounding tissues. Other common findings include loss of fibrillar structure, increased echogenicity, and the presence of calcifications or calcific deposits within the tendon. Doppler ultrasound may reveal increased blood flow within the affected area. These ultrasound findings are indicative of the pathological changes that occur in the patellar tendon due to chronic overuse and repetitive stress, leading to the development of tendinopathy.
Musculoskeletal ultrasound plays a crucial role in the evaluation of osteosarcoma by providing valuable information about the tumor's location, size, and characteristics. This imaging technique utilizes high-frequency sound waves to create real-time images of the musculoskeletal system, allowing for the detection of abnormalities in the bones and soft tissues. In the case of osteosarcoma, ultrasound can help identify the primary tumor site, assess the extent of local invasion, and determine the presence of metastases. Additionally, musculoskeletal ultrasound can aid in guiding biopsies and monitoring the response to treatment. By utilizing this non-invasive and cost-effective imaging modality, healthcare professionals can obtain detailed information about osteosarcoma, facilitating accurate diagnosis and treatment planning.
Musculoskeletal ultrasound has been found to be a valuable tool in detecting osteophytes in patients with osteoarthritis. Osteophytes, also known as bone spurs, are bony outgrowths that develop on the edges of bones in response to joint degeneration. By utilizing high-frequency sound waves, musculoskeletal ultrasound can provide detailed images of the affected joints, allowing healthcare professionals to visualize and identify the presence of osteophytes. This non-invasive imaging technique offers advantages such as real-time imaging, portability, and cost-effectiveness. Additionally, musculoskeletal ultrasound can assess other aspects of osteoarthritis, such as joint inflammation and synovial fluid abnormalities, providing a comprehensive evaluation of the disease. Overall, musculoskeletal ultrasound is a valuable diagnostic tool for detecting osteophytes in patients with osteoarthritis, aiding in the accurate assessment and management of this degenerative joint condition.