

Ultrasound guidance improves the accuracy of needle placement during medical procedures by providing real-time imaging of the target area. This allows healthcare professionals to visualize the needle as it is inserted, ensuring that it is accurately positioned. The ultrasound image provides detailed information about the surrounding structures, such as blood vessels and nerves, helping to avoid accidental puncture or damage. Additionally, ultrasound guidance allows for precise needle placement in difficult-to-access areas, reducing the risk of complications and improving the overall success rate of the procedure.
Using ultrasound guidance for central venous catheter placement offers several advantages. Firstly, it allows for real-time visualization of the target vein, ensuring accurate needle insertion. This reduces the risk of complications such as arterial puncture or pneumothorax. Secondly, ultrasound guidance enables healthcare professionals to assess the vein's size, depth, and patency, helping to select the most suitable site for catheter placement. This improves the success rate of the procedure and reduces the need for multiple attempts. Lastly, ultrasound guidance allows for the identification of potential complications, such as thrombosis or malpositioning of the catheter, facilitating prompt intervention and minimizing patient discomfort.
Over the last couple of years, we’ve brought you several courses focusing on Ultrasound Guided Injection Techniques. They’ve been extremely popular, and like our other courses, the feedback has been fantastic. One thing we’ve learnt along the way is that to get the most out of learning injection techniques, a solid grounding in MSK Ultrasound ...
Posted by on 2024-02-10
What a year 2023 was! We’ve loved bringing you courses covering US of the upper and lower limb, and US guided injections through the year. The mix of health professionals from all sorts of backgrounds (Doctors, Nurses, Physios, Sonographers to name a few) has been amazing to be part of. We’ve been humbled by your ...
Posted by on 2023-09-17
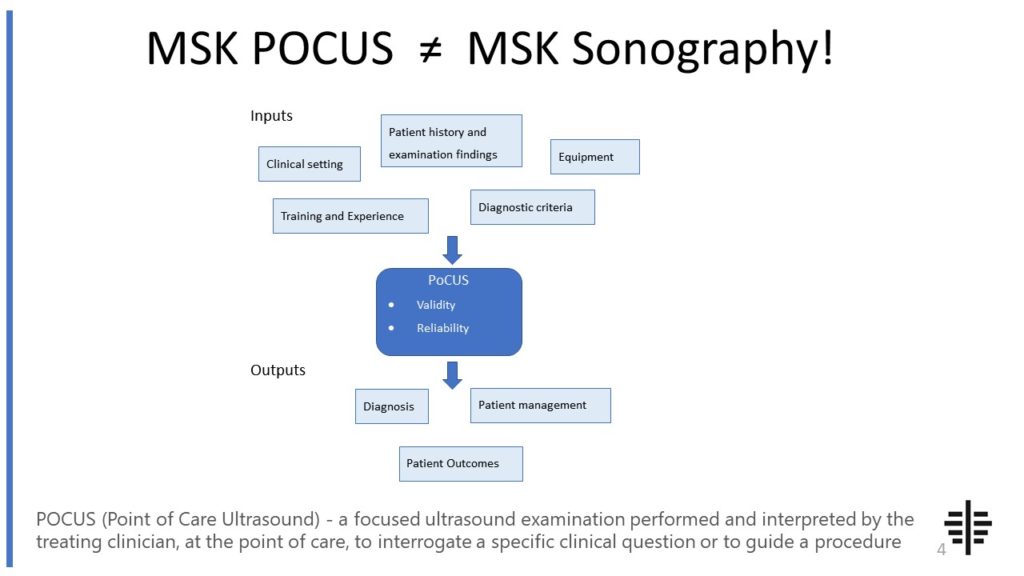
The POCUS process is very different to traditional US based in a radiology establishment. And POCUS practitioners need to be aware of those factors, unique to their particular situation, that influence diagnostic accuracy. That was the topic I presented at the plenary session of the NZAMM Annual Scientific Meeting in Wellington. A picture says 1000 ...
Posted by on 2022-10-04
We’re proud to announce that the New Zealand College of Musculoskeletal Medicine has endorsed our POCUS courses for CME and as part of vocational training. The NZCMM is responsible for setting the high standards and training of Specialist Musculoskeletal Medicine Physicians in New Zealand. NZCMM endorsement is an acknowledgement that our courses meet these standards. ...

Posted by on 2022-06-23
Ultrasound guidance plays a crucial role in the diagnosis and treatment of musculoskeletal conditions. It allows healthcare professionals to visualize the soft tissues, joints, tendons, and ligaments in real-time, providing valuable information about their structure and function. This helps in the accurate diagnosis of conditions such as tendonitis, bursitis, and ligament tears. Furthermore, ultrasound guidance can be used to guide therapeutic interventions, such as joint injections or aspirations. By visualizing the needle in real-time, healthcare professionals can ensure precise placement of medication or removal of fluid, improving the effectiveness of the treatment and reducing the risk of complications.

While ultrasound-guided procedures are generally considered safe, there are potential complications and risks associated with them. These include infection at the needle insertion site, bleeding, nerve injury, and allergic reactions to local anesthetics or contrast agents. It is important for healthcare professionals to follow strict aseptic techniques to minimize the risk of infection. Additionally, proper training and expertise in ultrasound-guided procedures are essential to reduce the risk of complications. Patients with certain medical conditions, such as bleeding disorders or allergies, may also have an increased risk of complications and should be carefully evaluated before undergoing ultrasound-guided procedures.
Yes, ultrasound guidance can be used for nerve blocks and regional anesthesia. It allows healthcare professionals to visualize the nerves and surrounding structures in real-time, ensuring accurate needle placement and delivery of medication. This improves the success rate of nerve blocks and regional anesthesia, reducing the risk of complications such as nerve injury or inadequate pain relief. Ultrasound guidance also allows for the identification of anatomical variations or abnormalities that may affect the procedure, enabling healthcare professionals to adapt their approach accordingly.

Ultrasound guidance enhances the safety and effectiveness of joint injections in several ways. Firstly, it allows healthcare professionals to visualize the joint space and surrounding structures, ensuring accurate needle placement. This reduces the risk of complications such as infection or damage to nearby structures. Secondly, ultrasound guidance enables the identification of joint effusions or synovial thickening, which may not be apparent on physical examination alone. This helps in determining the appropriate site for injection and improves the effectiveness of the treatment. Lastly, real-time visualization of the needle during joint injections allows for precise delivery of medication, maximizing its therapeutic effect.
While ultrasound guidance is a valuable tool in medical procedures, there are limitations and contraindications to its use. For example, ultrasound may not be suitable for patients with certain body habitus, such as obesity, as it may limit the quality of the images obtained. Additionally, ultrasound may not be effective in visualizing structures that are deep within the body or obscured by bone or air. In some cases, alternative imaging modalities, such as fluoroscopy or CT scan, may be more appropriate. Furthermore, patients with certain medical conditions, such as severe respiratory distress or unstable hemodynamics, may not be suitable candidates for ultrasound-guided procedures. It is important for healthcare professionals to carefully evaluate each patient's individual circumstances and consider the potential limitations and contraindications before using ultrasound guidance.

Musculoskeletal ultrasound plays a crucial role in the diagnosis of Morton's neuroma by providing detailed imaging of the affected area. This non-invasive imaging technique utilizes high-frequency sound waves to create real-time images of the musculoskeletal structures, including the foot. By using musculoskeletal ultrasound, healthcare professionals can visualize the neuroma, a benign growth of nerve tissue, in the intermetatarsal spaces of the foot. The ultrasound can accurately identify the size, location, and extent of the neuroma, allowing for a precise diagnosis. Additionally, musculoskeletal ultrasound can help differentiate Morton's neuroma from other conditions that may present with similar symptoms, such as stress fractures or bursitis. Overall, musculoskeletal ultrasound aids in the diagnosis of Morton's neuroma by providing valuable visual information that assists healthcare professionals in making an accurate and timely diagnosis.
Musculoskeletal ultrasound has the potential to differentiate between benign and malignant soft tissue tumors. This imaging technique utilizes high-frequency sound waves to produce detailed images of the musculoskeletal system, allowing for the evaluation of various soft tissue abnormalities. By assessing the characteristics of the tumor, such as size, shape, vascularity, and internal architecture, musculoskeletal ultrasound can provide valuable information that aids in distinguishing between benign and malignant tumors. Additionally, the use of Doppler ultrasound can assess blood flow within the tumor, which can be indicative of malignancy. However, it is important to note that while musculoskeletal ultrasound can provide valuable information, it is not always definitive in differentiating between benign and malignant soft tissue tumors. Therefore, further diagnostic tests, such as biopsy or magnetic resonance imaging (MRI), may be necessary for a conclusive diagnosis.
Musculoskeletal ultrasound plays a crucial role in diagnosing gout by providing valuable insights into the affected joints and surrounding tissues. This imaging technique utilizes high-frequency sound waves to create detailed images of the musculoskeletal system, allowing healthcare professionals to visualize the presence of urate crystals, a hallmark of gout. By examining the joints, tendons, and soft tissues, musculoskeletal ultrasound can detect the characteristic signs of gout, such as tophi (deposits of urate crystals) and synovial inflammation. Additionally, this diagnostic tool enables the assessment of joint damage and the identification of other potential causes of joint pain, ensuring an accurate diagnosis and appropriate treatment plan for individuals suspected of having gout.
Musculoskeletal ultrasound plays a crucial role in the diagnosis of peroneal tendon injuries by providing detailed imaging of the affected area. This imaging technique utilizes high-frequency sound waves to create real-time images of the musculoskeletal structures, allowing for the visualization of the peroneal tendons and surrounding tissues. By using musculoskeletal ultrasound, healthcare professionals can accurately assess the integrity of the peroneal tendons, identify any abnormalities or tears, and determine the extent of the injury. Additionally, this imaging modality enables the evaluation of adjacent structures such as the peroneal retinaculum and the presence of any associated inflammation or fluid accumulation. The use of musculoskeletal ultrasound in diagnosing peroneal tendon injuries enhances the accuracy of the diagnosis, aids in treatment planning, and facilitates timely intervention to promote optimal patient outcomes.
Musculoskeletal ultrasound can be a useful tool for diagnosing bursitis. Bursitis is an inflammatory condition that affects the bursae, which are small fluid-filled sacs that cushion the joints. Ultrasound imaging can help visualize the affected area and identify any abnormalities or inflammation in the bursa. It can also help differentiate bursitis from other conditions that may present with similar symptoms. By using musculoskeletal ultrasound, healthcare professionals can accurately diagnose bursitis and develop an appropriate treatment plan.
Musculoskeletal ultrasound can be a useful tool in the diagnosis of osteomyelitis. This imaging technique utilizes high-frequency sound waves to create detailed images of the musculoskeletal system, allowing for the visualization of bones, joints, and soft tissues. By examining these images, healthcare professionals can look for signs of infection, such as bone destruction, periosteal reaction, and abscess formation. Additionally, musculoskeletal ultrasound can help guide the placement of a needle for aspiration or biopsy, aiding in the collection of samples for further analysis. While musculoskeletal ultrasound is not the definitive diagnostic tool for osteomyelitis, it can provide valuable information that can support the diagnosis and inform treatment decisions.