

Ultrasound is a valuable tool in diagnosing hematomas because it allows for real-time visualization of the affected area. By using high-frequency sound waves, ultrasound can create detailed images of the soft tissues, including the hematoma. This imaging technique can help healthcare professionals determine the size, shape, and location of the hematoma, as well as assess its severity. Additionally, ultrasound can also provide information about the surrounding structures, such as blood vessels, which can be helpful in evaluating the potential complications associated with the hematoma.
There are several advantages of using ultrasound for detecting hematomas compared to other imaging techniques. Firstly, ultrasound is non-invasive and does not involve the use of ionizing radiation, making it a safer option for patients, especially those who may need repeated imaging. Secondly, ultrasound is readily available, portable, and relatively inexpensive compared to other imaging modalities like CT scans or MRI. This accessibility allows for quick and convenient evaluation of hematomas, particularly in emergency or outpatient settings. Lastly, ultrasound provides real-time imaging, allowing for dynamic assessment of the hematoma and the ability to visualize any changes that may occur during the examination.
Over the last couple of years, we’ve brought you several courses focusing on Ultrasound Guided Injection Techniques. They’ve been extremely popular, and like our other courses, the feedback has been fantastic. One thing we’ve learnt along the way is that to get the most out of learning injection techniques, a solid grounding in MSK Ultrasound ...
Posted by on 2024-02-10
What a year 2023 was! We’ve loved bringing you courses covering US of the upper and lower limb, and US guided injections through the year. The mix of health professionals from all sorts of backgrounds (Doctors, Nurses, Physios, Sonographers to name a few) has been amazing to be part of. We’ve been humbled by your ...
Posted by on 2023-09-17
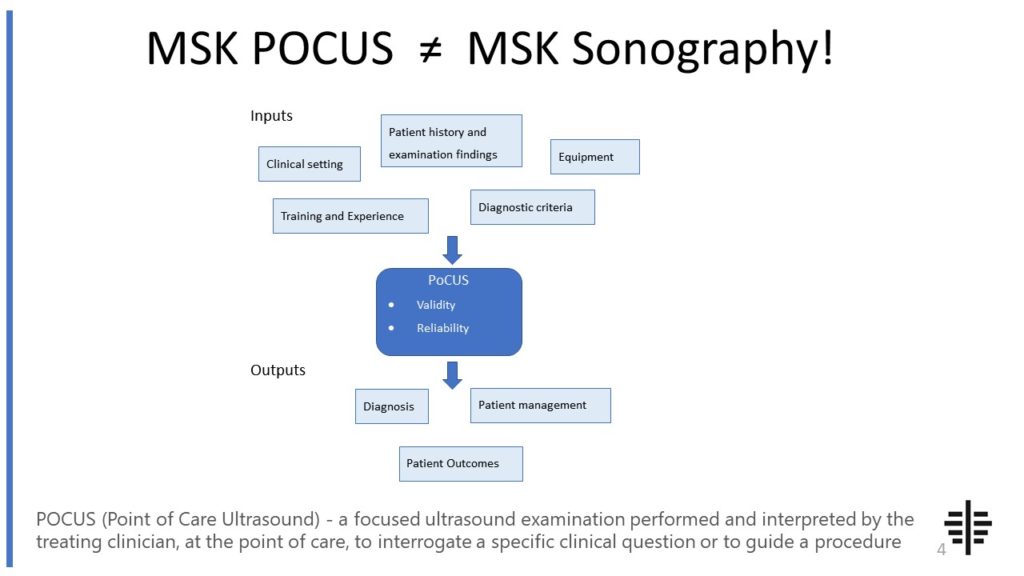
The POCUS process is very different to traditional US based in a radiology establishment. And POCUS practitioners need to be aware of those factors, unique to their particular situation, that influence diagnostic accuracy. That was the topic I presented at the plenary session of the NZAMM Annual Scientific Meeting in Wellington. A picture says 1000 ...
Posted by on 2022-10-04
We’re proud to announce that the New Zealand College of Musculoskeletal Medicine has endorsed our POCUS courses for CME and as part of vocational training. The NZCMM is responsible for setting the high standards and training of Specialist Musculoskeletal Medicine Physicians in New Zealand. NZCMM endorsement is an acknowledgement that our courses meet these standards. ...

Posted by on 2022-06-23
Ultrasound can accurately determine the size and location of a hematoma. By using ultrasound, healthcare professionals can measure the dimensions of the hematoma, including its length, width, and depth. This information is crucial in assessing the severity of the hematoma and monitoring its progression over time. Additionally, ultrasound can precisely locate the hematoma within the body, providing valuable information for treatment planning. By visualizing the hematoma in real-time, healthcare professionals can ensure accurate needle placement for procedures such as aspiration or drainage.

While ultrasound is a versatile imaging technique, there may be limitations or challenges in using it for hematomas in certain body areas. For example, hematomas located deep within the body or in areas with limited access may be more challenging to visualize accurately with ultrasound. Additionally, the presence of air or gas in the surrounding tissues can interfere with ultrasound imaging, making it difficult to obtain clear images. In such cases, other imaging modalities like CT scans or MRI may be necessary to provide a more comprehensive evaluation of the hematoma.
Ultrasound can differentiate between a hematoma and other similar conditions by assessing its characteristics on imaging. Hematomas typically appear as hypoechoic or anechoic areas on ultrasound, meaning they appear darker or without echoes compared to the surrounding tissues. This distinguishes them from other conditions that may have different echogenicity patterns. Additionally, the shape, size, and location of the hematoma can also provide clues to differentiate it from other masses or fluid collections. However, in some cases, further imaging or additional diagnostic tests may be required to confirm the diagnosis and rule out other potential causes.

Yes, ultrasound can be used to monitor the progression or healing of a hematoma over time. By performing serial ultrasound examinations, healthcare professionals can assess changes in the size, shape, and echogenicity of the hematoma. This allows for the evaluation of the hematoma's response to treatment or natural healing processes. Additionally, ultrasound can also help identify any complications that may arise during the healing process, such as infection or abscess formation. Regular ultrasound monitoring can provide valuable information for adjusting treatment plans and ensuring optimal patient care.
There are specific ultrasound techniques and settings that are recommended for evaluating hematomas. To assess a hematoma, healthcare professionals typically use a high-frequency linear transducer, which provides detailed imaging of the superficial soft tissues. Adjusting the gain and depth settings can optimize the visualization of the hematoma and surrounding structures. Additionally, using color Doppler can help assess the vascularity of the hematoma and identify any associated vascular injuries. By employing these techniques and settings, healthcare professionals can obtain accurate and comprehensive information about the hematoma, aiding in diagnosis and treatment decisions.

Frozen shoulder syndrome, also known as adhesive capsulitis, is a condition characterized by pain and stiffness in the shoulder joint. While ultrasound is not the primary diagnostic tool for frozen shoulder syndrome, it can provide valuable information about the underlying pathology. Typical ultrasound findings in patients with frozen shoulder syndrome include thickening and inflammation of the joint capsule, as well as the presence of adhesions and fibrosis within the capsule. Additionally, ultrasound may reveal a decrease in the volume of the synovial fluid and the presence of joint effusion. These findings are indicative of the inflammatory process and the development of scar tissue within the shoulder joint, contributing to the restricted range of motion and pain experienced by patients with frozen shoulder syndrome.
Musculoskeletal ultrasound plays a crucial role in diagnosing carpal tunnel syndrome by providing detailed imaging of the musculoskeletal structures in the wrist and hand. This non-invasive imaging technique allows healthcare professionals to visualize the median nerve, tendons, ligaments, and surrounding tissues in real-time. By assessing the size and shape of the median nerve, as well as any abnormalities such as swelling or compression, musculoskeletal ultrasound can help confirm the presence of carpal tunnel syndrome. Additionally, this imaging modality can also identify other potential causes of symptoms, such as tendonitis or ganglion cysts, ensuring an accurate diagnosis and appropriate treatment plan.
Musculoskeletal ultrasound has several limitations when it comes to assessing spinal cord compression. Firstly, the technique is highly operator-dependent, meaning that the accuracy of the results can vary depending on the skill and experience of the person performing the ultrasound. Additionally, musculoskeletal ultrasound is limited in its ability to visualize structures deep within the body, such as the spinal cord. This can make it challenging to accurately assess the extent and severity of spinal cord compression. Furthermore, musculoskeletal ultrasound may not be able to provide a comprehensive evaluation of the surrounding soft tissues and bony structures, which are important in determining the underlying cause of the compression. Therefore, while musculoskeletal ultrasound can be a useful tool in the initial assessment of spinal cord compression, it should be complemented with other imaging modalities, such as magnetic resonance imaging (MRI), for a more comprehensive evaluation.
Typical ultrasound findings in patients with patellar tendinopathy include thickening and irregularity of the patellar tendon, hypoechoic areas within the tendon indicating degeneration, neovascularization, and increased vascularity. The tendon may also appear hypoechoic or hyperechoic compared to the surrounding tissues. Other common findings include loss of fibrillar structure, increased echogenicity, and the presence of calcifications or calcific deposits within the tendon. Doppler ultrasound may reveal increased blood flow within the affected area. These ultrasound findings are indicative of the pathological changes that occur in the patellar tendon due to chronic overuse and repetitive stress, leading to the development of tendinopathy.
Musculoskeletal ultrasound plays a crucial role in the evaluation of osteosarcoma by providing valuable information about the tumor's location, size, and characteristics. This imaging technique utilizes high-frequency sound waves to create real-time images of the musculoskeletal system, allowing for the detection of abnormalities in the bones and soft tissues. In the case of osteosarcoma, ultrasound can help identify the primary tumor site, assess the extent of local invasion, and determine the presence of metastases. Additionally, musculoskeletal ultrasound can aid in guiding biopsies and monitoring the response to treatment. By utilizing this non-invasive and cost-effective imaging modality, healthcare professionals can obtain detailed information about osteosarcoma, facilitating accurate diagnosis and treatment planning.
Musculoskeletal ultrasound has been found to be a valuable tool in detecting osteophytes in patients with osteoarthritis. Osteophytes, also known as bone spurs, are bony outgrowths that develop on the edges of bones in response to joint degeneration. By utilizing high-frequency sound waves, musculoskeletal ultrasound can provide detailed images of the affected joints, allowing healthcare professionals to visualize and identify the presence of osteophytes. This non-invasive imaging technique offers advantages such as real-time imaging, portability, and cost-effectiveness. Additionally, musculoskeletal ultrasound can assess other aspects of osteoarthritis, such as joint inflammation and synovial fluid abnormalities, providing a comprehensive evaluation of the disease. Overall, musculoskeletal ultrasound is a valuable diagnostic tool for detecting osteophytes in patients with osteoarthritis, aiding in the accurate assessment and management of this degenerative joint condition.