

Ultrasound imaging plays a crucial role in the diagnosis of musculoskeletal conditions in geriatric patients. It allows healthcare professionals to visualize and assess the soft tissues, joints, tendons, and ligaments in real-time. This imaging modality can help identify various musculoskeletal abnormalities such as fractures, sprains, tears, and inflammation. Additionally, ultrasound can provide valuable information about the extent and severity of the condition, aiding in treatment planning and monitoring the progress of the patient's condition. Overall, ultrasound imaging is a non-invasive and safe tool that assists in the accurate diagnosis of musculoskeletal conditions in geriatric patients.
There are several advantages of using ultrasound over other imaging modalities in geriatric musculoskeletal imaging. Firstly, ultrasound is a non-ionizing imaging technique, which means it does not expose patients to harmful radiation. This is particularly beneficial for geriatric patients who may already have compromised health and are more susceptible to the adverse effects of radiation. Secondly, ultrasound is portable and readily available, allowing for convenient bedside examinations in geriatric patients who may have mobility limitations. Additionally, ultrasound provides real-time imaging, allowing for dynamic assessment of musculoskeletal structures during movement. This can be especially useful in evaluating joint function and detecting abnormalities that may not be apparent in static images. Overall, ultrasound offers advantages in terms of safety, accessibility, and dynamic imaging capabilities in geriatric musculoskeletal imaging.
Over the last couple of years, we’ve brought you several courses focusing on Ultrasound Guided Injection Techniques. They’ve been extremely popular, and like our other courses, the feedback has been fantastic. One thing we’ve learnt along the way is that to get the most out of learning injection techniques, a solid grounding in MSK Ultrasound ...
Posted by on 2024-02-10
What a year 2023 was! We’ve loved bringing you courses covering US of the upper and lower limb, and US guided injections through the year. The mix of health professionals from all sorts of backgrounds (Doctors, Nurses, Physios, Sonographers to name a few) has been amazing to be part of. We’ve been humbled by your ...
Posted by on 2023-09-17
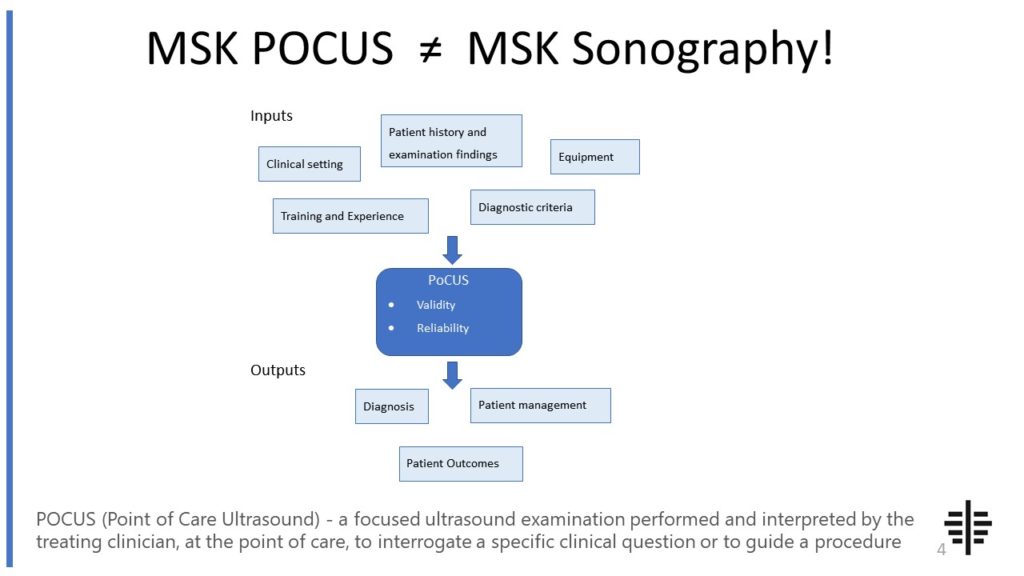
The POCUS process is very different to traditional US based in a radiology establishment. And POCUS practitioners need to be aware of those factors, unique to their particular situation, that influence diagnostic accuracy. That was the topic I presented at the plenary session of the NZAMM Annual Scientific Meeting in Wellington. A picture says 1000 ...
Posted by on 2022-10-04
We’re proud to announce that the New Zealand College of Musculoskeletal Medicine has endorsed our POCUS courses for CME and as part of vocational training. The NZCMM is responsible for setting the high standards and training of Specialist Musculoskeletal Medicine Physicians in New Zealand. NZCMM endorsement is an acknowledgement that our courses meet these standards. ...

Posted by on 2022-06-23
Despite its many benefits, ultrasound does have limitations in detecting certain musculoskeletal abnormalities in geriatric patients. One limitation is the limited penetration depth of ultrasound waves, which may hinder the visualization of deep structures such as bones and joints in obese or heavily muscled individuals. Additionally, ultrasound may not be as effective in detecting subtle abnormalities or small lesions compared to other imaging modalities like magnetic resonance imaging (MRI). Furthermore, the operator's skill and experience can significantly impact the accuracy and interpretation of ultrasound images. Therefore, it is important to consider these limitations and potentially complement ultrasound with other imaging modalities when necessary to ensure a comprehensive evaluation of musculoskeletal abnormalities in geriatric patients.

Ultrasound-guided intervention plays a crucial role in improving the accuracy and efficacy of treatments for musculoskeletal conditions in geriatric patients. By using ultrasound imaging to guide procedures such as joint injections, aspirations, and biopsies, healthcare professionals can ensure precise needle placement and target the specific area of concern. This reduces the risk of complications and increases the success rate of the intervention. Additionally, real-time visualization provided by ultrasound allows for immediate feedback during the procedure, enabling adjustments to be made as needed. Overall, ultrasound-guided intervention enhances the safety and effectiveness of treatments for musculoskeletal conditions in geriatric patients, leading to improved patient outcomes.
Ultrasound is effective in evaluating a wide range of musculoskeletal conditions in geriatric patients. Some common conditions that can be effectively evaluated using ultrasound include osteoarthritis, tendinopathies, rotator cuff tears, carpal tunnel syndrome, and bursitis. Ultrasound can provide detailed information about the integrity of tendons, ligaments, and muscles, as well as detect signs of inflammation, fluid accumulation, or structural abnormalities. This allows for accurate diagnosis, treatment planning, and monitoring of these conditions in geriatric patients. The real-time imaging capabilities of ultrasound also make it a valuable tool in assessing joint function and guiding interventions such as injections or aspirations.

The use of ultrasound in geriatric musculoskeletal imaging contributes significantly to the early detection and prevention of age-related musculoskeletal disorders. By allowing healthcare professionals to visualize and assess the musculoskeletal system in real-time, ultrasound can detect subtle changes and abnormalities at an early stage. This early detection enables timely intervention and treatment, potentially preventing the progression of musculoskeletal disorders and reducing the risk of complications. Furthermore, ultrasound can aid in the identification of modifiable risk factors such as muscle imbalances or joint misalignments, allowing for targeted interventions and preventive measures. Overall, ultrasound plays a crucial role in promoting early detection and prevention of age-related musculoskeletal disorders in geriatric patients.
Performing ultrasound examinations on geriatric patients with musculoskeletal complaints requires careful consideration of several key factors and challenges. Firstly, the operator must be skilled and experienced in geriatric musculoskeletal imaging to ensure accurate and reliable results. Geriatric patients may have unique anatomical variations, comorbidities, or mobility limitations that can affect the imaging process. Therefore, the operator must adapt the examination technique and settings accordingly. Additionally, patient cooperation and comfort are essential, as geriatric patients may experience pain or discomfort during the examination. Proper positioning and communication techniques should be employed to ensure a positive patient experience. Lastly, the interpretation of ultrasound images in geriatric patients may require additional expertise due to age-related changes in musculoskeletal structures. Therefore, collaboration between radiologists, orthopedic specialists, and geriatric healthcare professionals is crucial to ensure comprehensive and accurate diagnosis and management of musculoskeletal conditions in geriatric patients.

Musculoskeletal ultrasound offers several advantages over clinical examination when diagnosing joint effusions. Firstly, ultrasound allows for real-time visualization of the joint space, providing a detailed assessment of the extent and location of the effusion. This enables the clinician to accurately measure the size of the effusion and monitor its progression over time. Additionally, ultrasound can help differentiate between different types of effusions, such as inflammatory or infectious, by assessing the presence of synovial thickening or debris within the joint. Furthermore, ultrasound-guided aspiration of the effusion can be performed, ensuring accurate targeting and minimizing the risk of complications. Overall, musculoskeletal ultrasound enhances the diagnostic accuracy and precision in evaluating joint effusions, leading to improved patient management and outcomes.
Musculoskeletal ultrasound has the potential to detect early changes in osteoarthritic joints. This imaging technique utilizes high-frequency sound waves to create detailed images of the musculoskeletal system, including the joints. By examining the joint structures, such as the cartilage, synovium, and subchondral bone, musculoskeletal ultrasound can identify early signs of osteoarthritis, such as joint space narrowing, cartilage thinning, and synovial inflammation. Additionally, musculoskeletal ultrasound can assess the presence of joint effusion, osteophytes, and subchondral cysts, which are common features of osteoarthritic joints. The use of musculoskeletal ultrasound in detecting these early changes in osteoarthritic joints can aid in the early diagnosis and management of osteoarthritis, potentially leading to better outcomes for patients.
Musculoskeletal ultrasound plays a crucial role in the assessment of inflammatory myopathies by providing valuable information about the extent and severity of muscle inflammation. This imaging technique allows for the visualization of muscle architecture, including the presence of edema, muscle fiber disruption, and fatty infiltration. Additionally, musculoskeletal ultrasound can detect characteristic findings such as muscle thickening, hypoechoic areas, and increased vascularity, which are indicative of inflammatory myopathies. By accurately assessing the degree of muscle involvement and identifying specific patterns of inflammation, musculoskeletal ultrasound aids in the diagnosis and monitoring of these conditions, guiding treatment decisions and assessing response to therapy.
Musculoskeletal ultrasound is a valuable imaging modality that can aid in the diagnosis of avascular necrosis of bone. It utilizes high-frequency sound waves to produce detailed images of the musculoskeletal system, allowing for the visualization of bone structures and surrounding soft tissues. While it is not the gold standard for diagnosing avascular necrosis, musculoskeletal ultrasound can provide valuable information about the blood supply to the affected bone and detect early signs of necrosis. Additionally, it can help differentiate avascular necrosis from other conditions that may present with similar symptoms. However, it is important to note that the accuracy of the diagnosis depends on the skill and experience of the ultrasound operator. Therefore, musculoskeletal ultrasound should be used in conjunction with other imaging modalities, such as magnetic resonance imaging (MRI), to ensure a comprehensive and accurate diagnosis of avascular necrosis of bone.
Musculoskeletal ultrasound is a valuable tool for assessing cervical spine pathology, but it does have some limitations. One limitation is that it may not provide a comprehensive view of the entire cervical spine. Due to the limited field of view, it may be challenging to visualize structures that are located deep within the spine or obscured by bone or other structures. Additionally, musculoskeletal ultrasound may not be able to accurately assess certain pathologies, such as fractures or tumors, which may require more advanced imaging techniques like CT or MRI. Another limitation is that the operator's skill and experience can greatly impact the accuracy and interpretation of the ultrasound images. Inexperienced operators may struggle to identify and properly assess specific cervical spine pathologies. Furthermore, patient factors such as obesity or limited range of motion can also affect the quality of the ultrasound images and make it more challenging to obtain accurate results. Overall, while musculoskeletal ultrasound can be a useful tool for assessing cervical spine pathology, it is important to consider its limitations and use it in conjunction with other imaging modalities when necessary.