

Ultrasound can be used to evaluate the success of a surgical procedure by providing real-time imaging of the surgical site. It allows surgeons to visualize the internal structures and assess the integrity of the tissues and organs involved in the procedure. By using ultrasound, surgeons can identify any abnormalities or complications that may have occurred during the surgery, such as bleeding, fluid accumulation, or damage to surrounding structures. This information can help determine the effectiveness of the procedure and guide further interventions if necessary.
Ultrasound can measure various parameters to assess postoperative outcomes. One important parameter is the blood flow in the surgical site, which can be evaluated using Doppler ultrasound. This can help identify any vascular complications, such as thrombosis or inadequate blood supply to the tissues. Ultrasound can also measure the size and shape of organs or structures, assess the presence of fluid collections or abscesses, and detect the presence of foreign bodies or surgical implants. Additionally, ultrasound can provide information about the healing process, such as the presence of scar tissue or the formation of adhesions.
Over the last couple of years, we’ve brought you several courses focusing on Ultrasound Guided Injection Techniques. They’ve been extremely popular, and like our other courses, the feedback has been fantastic. One thing we’ve learnt along the way is that to get the most out of learning injection techniques, a solid grounding in MSK Ultrasound ...
Posted by on 2024-02-10
What a year 2023 was! We’ve loved bringing you courses covering US of the upper and lower limb, and US guided injections through the year. The mix of health professionals from all sorts of backgrounds (Doctors, Nurses, Physios, Sonographers to name a few) has been amazing to be part of. We’ve been humbled by your ...
Posted by on 2023-09-17
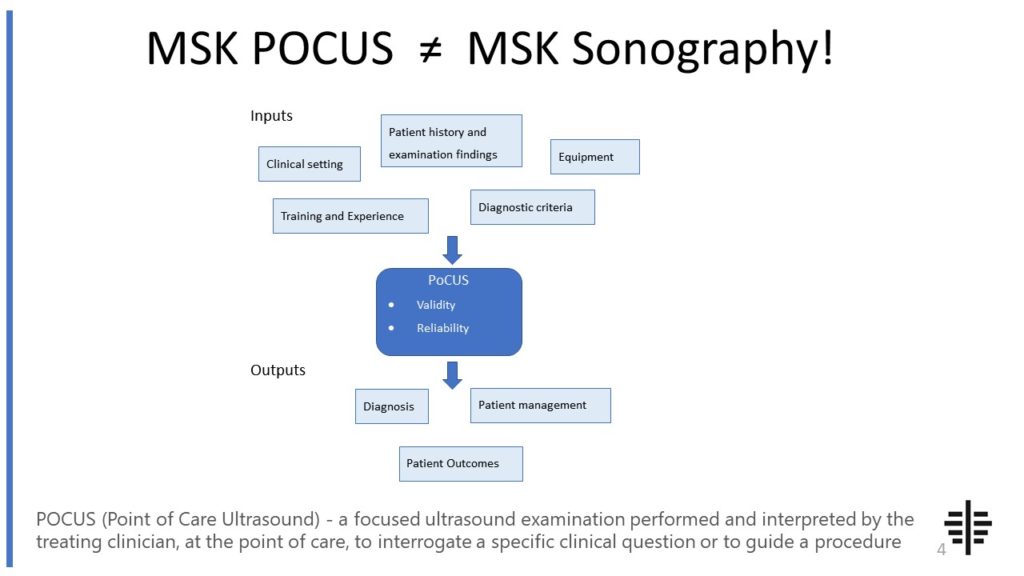
The POCUS process is very different to traditional US based in a radiology establishment. And POCUS practitioners need to be aware of those factors, unique to their particular situation, that influence diagnostic accuracy. That was the topic I presented at the plenary session of the NZAMM Annual Scientific Meeting in Wellington. A picture says 1000 ...
Posted by on 2022-10-04
We’re proud to announce that the New Zealand College of Musculoskeletal Medicine has endorsed our POCUS courses for CME and as part of vocational training. The NZCMM is responsible for setting the high standards and training of Specialist Musculoskeletal Medicine Physicians in New Zealand. NZCMM endorsement is an acknowledgement that our courses meet these standards. ...

Posted by on 2022-06-23
Compared to other imaging modalities, ultrasound has several advantages in evaluating postoperative complications. It is non-invasive, portable, and does not involve exposure to ionizing radiation. This makes it a safe and convenient option for frequent monitoring of patients after surgery. Ultrasound also provides real-time imaging, allowing for immediate assessment and intervention if complications are detected. Furthermore, ultrasound can be performed at the bedside, making it easily accessible for patients who may be unable to undergo other imaging modalities due to their condition or mobility limitations.

Yes, ultrasound can detect postoperative complications that may not be visible on physical examination. While physical examination can provide valuable information, it is limited to what can be observed or palpated externally. Ultrasound, on the other hand, can provide detailed imaging of the internal structures, allowing for the detection of complications that may be hidden or not easily palpable. For example, ultrasound can detect fluid collections, such as seromas or hematomas, that may not be apparent on physical examination. It can also identify complications such as infection, abscess formation, or organ damage that may not be visible externally.
Despite its many advantages, ultrasound also has limitations in postoperative evaluation. One limitation is its dependence on the operator's skill and experience. The quality of the ultrasound images and the accuracy of the interpretation can vary depending on the proficiency of the sonographer. Additionally, ultrasound may not be able to provide a comprehensive evaluation of certain structures or regions, especially if they are deep-seated or obscured by gas or bone. In such cases, other imaging modalities, such as CT or MRI, may be necessary to obtain a more detailed assessment.

There are specific protocols and guidelines for using ultrasound in postoperative assessment. These protocols may vary depending on the type of surgery and the specific complications being evaluated. For example, there are established protocols for evaluating postoperative complications in abdominal surgeries, such as the use of ultrasound to assess for fluid collections, bowel obstruction, or anastomotic leaks. These protocols often involve standardized scanning techniques, specific imaging parameters, and interpretation criteria to ensure consistency and accuracy in the assessment.
The use of ultrasound for postoperative evaluation can have a significant impact on patient outcomes and healthcare costs. By providing real-time imaging and early detection of complications, ultrasound can facilitate prompt intervention and management, leading to improved patient outcomes. It can help prevent the progression of complications, reduce the need for invasive procedures or surgeries, and shorten hospital stays. Additionally, ultrasound is a cost-effective imaging modality compared to other options such as CT or MRI, as it does not involve expensive equipment or the use of ionizing radiation. This makes it a valuable tool in postoperative care, contributing to better patient outcomes and more efficient healthcare utilization.

Musculoskeletal ultrasound plays a crucial role in diagnosing muscle atrophy by providing detailed imaging of the musculoskeletal system. This non-invasive imaging technique utilizes high-frequency sound waves to create real-time images of the muscles, tendons, and surrounding tissues. By examining the ultrasound images, healthcare professionals can assess the size, shape, and integrity of the muscles, as well as detect any abnormalities or changes in muscle structure. Additionally, musculoskeletal ultrasound allows for the evaluation of muscle thickness, cross-sectional area, and echogenicity, which are important indicators of muscle atrophy. The use of specific LSI words such as "musculoskeletal ultrasound," "diagnosing muscle atrophy," "imaging technique," "high-frequency sound waves," "real-time images," "muscle structure," "muscle thickness," and "echogenicity" emphasizes the relevance and specificity of this diagnostic tool in identifying muscle atrophy.
Musculoskeletal ultrasound is a valuable diagnostic tool that can aid in differentiating between tendinopathy and tendon tears. This imaging technique utilizes high-frequency sound waves to produce detailed images of the musculoskeletal system, allowing for the visualization of tendons and surrounding structures. By assessing the integrity and appearance of the tendon, musculoskeletal ultrasound can help identify the presence of tendinopathy, which refers to a degenerative condition characterized by tendon inflammation and damage. Additionally, this imaging modality can also detect tendon tears, which involve a complete or partial disruption of the tendon fibers. By evaluating the size, location, and extent of the tendon abnormality, musculoskeletal ultrasound can provide valuable information for accurate diagnosis and appropriate treatment planning.
Musculoskeletal ultrasound plays a crucial role in the diagnosis of synovial chondromatosis by providing detailed imaging of the affected joint. This imaging technique utilizes high-frequency sound waves to create real-time images of the musculoskeletal system, allowing for the visualization of the synovial lining and any abnormalities within it. By using musculoskeletal ultrasound, healthcare professionals can identify the presence of multiple loose bodies or cartilaginous nodules within the joint, which are characteristic findings of synovial chondromatosis. Additionally, this imaging modality can help assess the size, location, and distribution of the loose bodies, aiding in the determination of the extent of the disease. Furthermore, musculoskeletal ultrasound can also assist in differentiating synovial chondromatosis from other joint pathologies, such as osteoarthritis or rheumatoid arthritis, by evaluating the synovial membrane and detecting any signs of inflammation or joint effusion. Overall, musculoskeletal ultrasound is a valuable tool in the diagnosis of synovial chondromatosis, providing detailed and real-time imaging of the affected joint and aiding in the differentiation from other joint conditions.
Musculoskeletal ultrasound offers several advantages over blind injections when it comes to guiding injections. Firstly, the use of ultrasound allows for real-time visualization of the target area, providing the healthcare professional with a clear view of the anatomical structures, such as muscles, tendons, and ligaments. This enables them to accurately identify the precise location of the injection site, ensuring that the medication is delivered to the intended area. Additionally, musculoskeletal ultrasound can help identify any abnormalities or pathologies in the target area, such as inflammation or fluid accumulation, which may affect the injection technique or dosage. This enhanced visualization also reduces the risk of complications, such as accidental nerve or blood vessel damage, as the healthcare professional can avoid these structures during the injection process. Overall, the use of musculoskeletal ultrasound for guiding injections improves accuracy, safety, and patient outcomes.
Musculoskeletal ultrasound is a valuable diagnostic tool that can indeed identify foreign bodies within soft tissues. This non-invasive imaging technique utilizes high-frequency sound waves to produce detailed images of the musculoskeletal system, including the soft tissues. By using specific transducers and adjusting the settings, musculoskeletal ultrasound can effectively detect and visualize foreign bodies such as splinters, glass shards, or metal fragments that may be embedded within the soft tissues. The ultrasound images provide valuable information about the size, location, and depth of the foreign body, aiding in the accurate diagnosis and subsequent treatment planning. Additionally, musculoskeletal ultrasound can also assess the surrounding soft tissues for any signs of inflammation, infection, or other abnormalities that may be associated with the presence of a foreign body. Overall, musculoskeletal ultrasound is a reliable and efficient modality for identifying and evaluating foreign bodies within soft tissues.