

Ultrasound can be used to diagnose enthesopathy by visualizing the affected area and assessing the integrity of the enthesis, which is the site where a tendon or ligament attaches to the bone. Ultrasound can provide real-time imaging of the enthesis, allowing for the detection of abnormalities such as thickening, calcifications, or erosions. Additionally, ultrasound can assess the surrounding soft tissues and identify any signs of inflammation or fluid accumulation, which are common features of enthesopathy. By using ultrasound, healthcare professionals can accurately diagnose enthesopathy and determine the extent of the condition.
There are several advantages of using ultrasound over other imaging techniques for detecting enthesopathy. Firstly, ultrasound is non-invasive and does not involve exposure to ionizing radiation, making it a safe option for repeated imaging and monitoring. Secondly, ultrasound provides real-time imaging, allowing for dynamic assessment of the enthesis during movement or stress. This can help in identifying subtle abnormalities that may not be evident in static images. Additionally, ultrasound is relatively inexpensive and widely available, making it a cost-effective option for diagnosing and monitoring enthesopathy. Overall, ultrasound offers a combination of safety, real-time imaging, and accessibility, making it a valuable tool in the detection of enthesopathy.
Over the last couple of years, we’ve brought you several courses focusing on Ultrasound Guided Injection Techniques. They’ve been extremely popular, and like our other courses, the feedback has been fantastic. One thing we’ve learnt along the way is that to get the most out of learning injection techniques, a solid grounding in MSK Ultrasound ...
Posted by on 2024-02-10
What a year 2023 was! We’ve loved bringing you courses covering US of the upper and lower limb, and US guided injections through the year. The mix of health professionals from all sorts of backgrounds (Doctors, Nurses, Physios, Sonographers to name a few) has been amazing to be part of. We’ve been humbled by your ...
Posted by on 2023-09-17
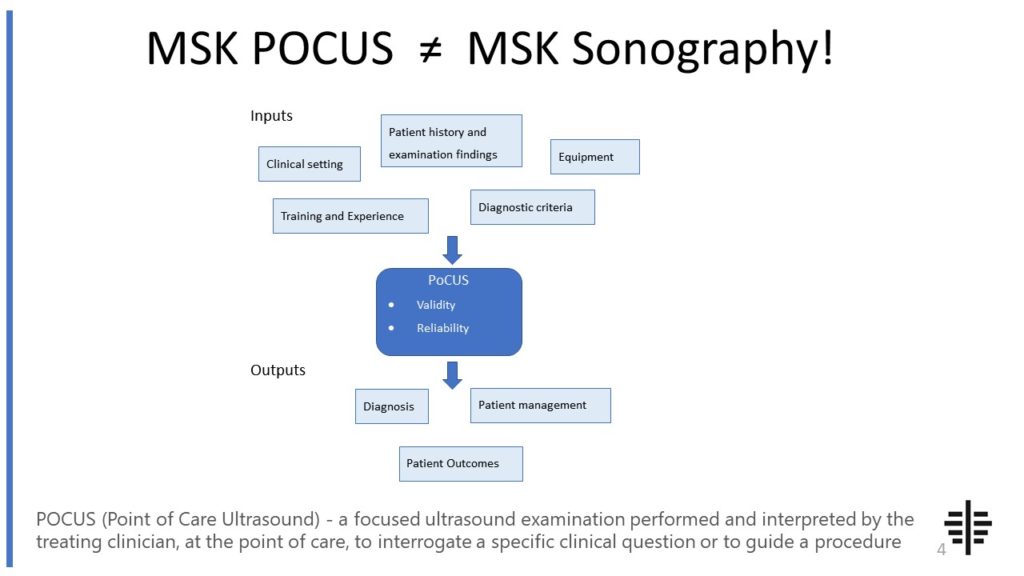
The POCUS process is very different to traditional US based in a radiology establishment. And POCUS practitioners need to be aware of those factors, unique to their particular situation, that influence diagnostic accuracy. That was the topic I presented at the plenary session of the NZAMM Annual Scientific Meeting in Wellington. A picture says 1000 ...
Posted by on 2022-10-04
We’re proud to announce that the New Zealand College of Musculoskeletal Medicine has endorsed our POCUS courses for CME and as part of vocational training. The NZCMM is responsible for setting the high standards and training of Specialist Musculoskeletal Medicine Physicians in New Zealand. NZCMM endorsement is an acknowledgement that our courses meet these standards. ...

Posted by on 2022-06-23
Specific ultrasound findings that indicate the presence of enthesopathy include thickening of the enthesis, irregularity or fragmentation of the bone surface, calcifications within the enthesis, and signs of inflammation such as increased blood flow or fluid accumulation. The presence of these findings can suggest the presence of enthesopathy and help differentiate it from other conditions. Additionally, ultrasound can assess the surrounding soft tissues for signs of inflammation, such as increased vascularity or swelling. By evaluating these specific ultrasound findings, healthcare professionals can make an accurate diagnosis of enthesopathy.

Ultrasound can differentiate between different types of enthesopathy to some extent. For example, in calcific enthesopathy, ultrasound can detect the presence of calcifications within the enthesis, which are characteristic of this condition. Similarly, in reactive enthesopathy, ultrasound may show signs of inflammation such as increased blood flow or fluid accumulation. However, it is important to note that ultrasound findings alone may not be sufficient to differentiate between all types of enthesopathy, and additional imaging or clinical information may be required for a definitive diagnosis. Therefore, while ultrasound can provide valuable information, it is often used in conjunction with other diagnostic tools to differentiate between different types of enthesopathy.
Ultrasound-guided treatment, such as ultrasound-guided injections, can help in managing enthesopathy by providing accurate and targeted delivery of medication to the affected area. By using ultrasound to visualize the enthesis and surrounding structures, healthcare professionals can precisely guide the needle to the desired location, ensuring that the medication is delivered directly to the site of pathology. This can improve the effectiveness of treatment and reduce the risk of complications. Additionally, ultrasound-guided injections can help in monitoring the response to treatment by allowing for real-time visualization of the enthesis and assessing any changes in the condition. Overall, ultrasound-guided treatment plays a valuable role in the management of enthesopathy by enhancing the accuracy and efficacy of interventions.

While ultrasound is a valuable tool for diagnosing and monitoring enthesopathy, there are some limitations and challenges associated with its use. One limitation is the operator-dependency of ultrasound, as the quality of the images and interpretation can vary depending on the skill and experience of the healthcare professional performing the examination. Additionally, ultrasound may not be able to visualize deep-seated entheses or structures that are obscured by overlying bone or gas-filled structures. Furthermore, ultrasound may not provide a comprehensive assessment of the entire musculoskeletal system, and additional imaging modalities such as MRI may be required for a more detailed evaluation. Despite these limitations, ultrasound remains a valuable tool in the diagnosis and monitoring of enthesopathy.
The potential future developments in ultrasound technology for the assessment of enthesopathy include advancements in image resolution, the development of specialized probes or transducers for specific anatomical regions, and the integration of advanced imaging techniques such as elastography or contrast-enhanced ultrasound. These developments can further improve the accuracy and diagnostic capabilities of ultrasound in detecting and characterizing enthesopathy. Additionally, the use of artificial intelligence and machine learning algorithms may help in automating the analysis of ultrasound images and improving the efficiency and consistency of diagnosis. Overall, the future of ultrasound technology holds promise for further enhancing its role in the assessment of enthesopathy.

In musculoskeletal ultrasound of patients with rheumatoid arthritis, typical findings include synovial hypertrophy, joint effusion, and power Doppler signal. Synovial hypertrophy refers to the thickening of the synovial lining of the joints, which is a characteristic feature of rheumatoid arthritis. Joint effusion, or the accumulation of fluid within the joint space, is commonly observed in patients with this condition. Power Doppler signal, which detects blood flow within the synovium, is often increased in rheumatoid arthritis due to the inflammation and increased vascularity associated with the disease. Other findings may include erosions, tenosynovitis, and bursitis, which are indicative of the destructive nature of rheumatoid arthritis on the musculoskeletal system. Overall, musculoskeletal ultrasound plays a valuable role in the assessment and monitoring of rheumatoid arthritis, providing important information about disease activity and progression.
Osteitis pubis is a condition characterized by inflammation of the pubic symphysis and surrounding structures. When evaluating patients with osteitis pubis using musculoskeletal ultrasound, typical findings may include thickening and irregularity of the pubic symphysis, increased vascularity in the affected area, and the presence of fluid collections or edema. Additionally, ultrasound may reveal tendon abnormalities, such as tendonitis or tears, in the adjacent muscles, such as the adductor muscles or rectus abdominis. The ultrasound may also show signs of bursitis or inflammation of the bursae surrounding the pubic symphysis. These findings are important in diagnosing and monitoring the progression of osteitis pubis, as well as guiding treatment decisions.
Musculoskeletal ultrasound plays a crucial role in the evaluation of soft tissue masses by providing detailed imaging of the affected area. This imaging technique utilizes high-frequency sound waves to create real-time images of the soft tissues, allowing for the identification and characterization of masses. By visualizing the size, shape, location, and internal structure of the mass, musculoskeletal ultrasound aids in determining the nature of the lesion, such as whether it is a benign or malignant tumor, a cyst, or an abscess. Additionally, musculoskeletal ultrasound can assess the vascularity of the mass by utilizing Doppler imaging, which helps in differentiating between solid and cystic lesions. Furthermore, this imaging modality allows for dynamic evaluation, enabling the assessment of the mass during movement or stress maneuvers, which can provide valuable information about its behavior and potential impact on nearby structures. Overall, musculoskeletal ultrasound is an invaluable tool in the assessment of soft tissue masses, aiding in accurate diagnosis and guiding appropriate management decisions.
Musculoskeletal ultrasound has proven to be a valuable tool in identifying synovitis in patients with inflammatory arthritis. This imaging technique utilizes high-frequency sound waves to produce detailed images of the musculoskeletal system, allowing for the visualization of synovial inflammation. By assessing the synovial membrane and joint space, musculoskeletal ultrasound can detect signs of synovitis, such as synovial thickening, increased vascularity, and effusion. Additionally, this modality enables the assessment of other related features, including erosions, tenosynovitis, and bursitis, providing a comprehensive evaluation of the inflammatory process. The use of musculoskeletal ultrasound in the diagnosis and monitoring of synovitis in patients with inflammatory arthritis has shown promising results, offering a non-invasive and cost-effective alternative to other imaging modalities.
Performing musculoskeletal ultrasound on obese patients presents several technical challenges. One of the main challenges is the increased depth of penetration required to visualize the musculoskeletal structures due to the thicker subcutaneous fat layer. This can result in reduced image quality and difficulty in identifying anatomical landmarks. Additionally, the increased attenuation of sound waves in obese patients can lead to decreased signal strength and decreased resolution of the ultrasound images. The larger body habitus of obese patients can also make it more challenging to position the ultrasound probe correctly and maintain adequate contact with the skin. Furthermore, the increased adipose tissue can cause acoustic shadowing, making it difficult to visualize structures that lie deep to the fat layer. These technical challenges highlight the importance of using appropriate ultrasound settings, selecting the appropriate transducer, and employing proper scanning techniques to optimize image quality and diagnostic accuracy in musculoskeletal ultrasound examinations of obese patients.
Musculoskeletal ultrasound has several limitations when it comes to assessing spinal tumors. Firstly, the technique is highly operator-dependent, meaning that the accuracy and reliability of the results can vary depending on the skill and experience of the sonographer. Additionally, musculoskeletal ultrasound has limited penetration through bone, which can make it difficult to visualize tumors that are located deep within the spine or surrounded by bony structures. Furthermore, the resolution of musculoskeletal ultrasound may not be sufficient to accurately characterize the size, shape, and extent of spinal tumors, especially in cases where there is significant surrounding tissue or bone interference. Lastly, musculoskeletal ultrasound may not be able to differentiate between benign and malignant tumors, as it primarily provides information about the anatomical features of the tumor rather than its cellular or molecular characteristics.