

Ultrasound is a highly accurate imaging technique for diagnosing tendon tears. Studies have shown that ultrasound has a sensitivity of over 90% and a specificity of over 95% in detecting tendon tears. This means that ultrasound is able to accurately identify the presence of a tendon tear in the majority of cases, and it also has a low rate of false positives, reducing the chances of misdiagnosis. Ultrasound can provide detailed images of the tendon structure, allowing for a thorough evaluation of the tear and its severity.
There are several advantages of using ultrasound for tendon tear diagnosis compared to other imaging techniques. Firstly, ultrasound is non-invasive and does not involve exposure to ionizing radiation, making it a safer option for patients. Additionally, ultrasound is a real-time imaging technique, allowing for dynamic assessment of the tendon during movement. This can be particularly useful in diagnosing tendon tears that may only be evident during certain movements or positions. Ultrasound is also relatively inexpensive and widely available, making it a cost-effective option for tendon tear diagnosis.
Over the last couple of years, we’ve brought you several courses focusing on Ultrasound Guided Injection Techniques. They’ve been extremely popular, and like our other courses, the feedback has been fantastic. One thing we’ve learnt along the way is that to get the most out of learning injection techniques, a solid grounding in MSK Ultrasound ...
Posted by on 2024-02-10
What a year 2023 was! We’ve loved bringing you courses covering US of the upper and lower limb, and US guided injections through the year. The mix of health professionals from all sorts of backgrounds (Doctors, Nurses, Physios, Sonographers to name a few) has been amazing to be part of. We’ve been humbled by your ...
Posted by on 2023-09-17
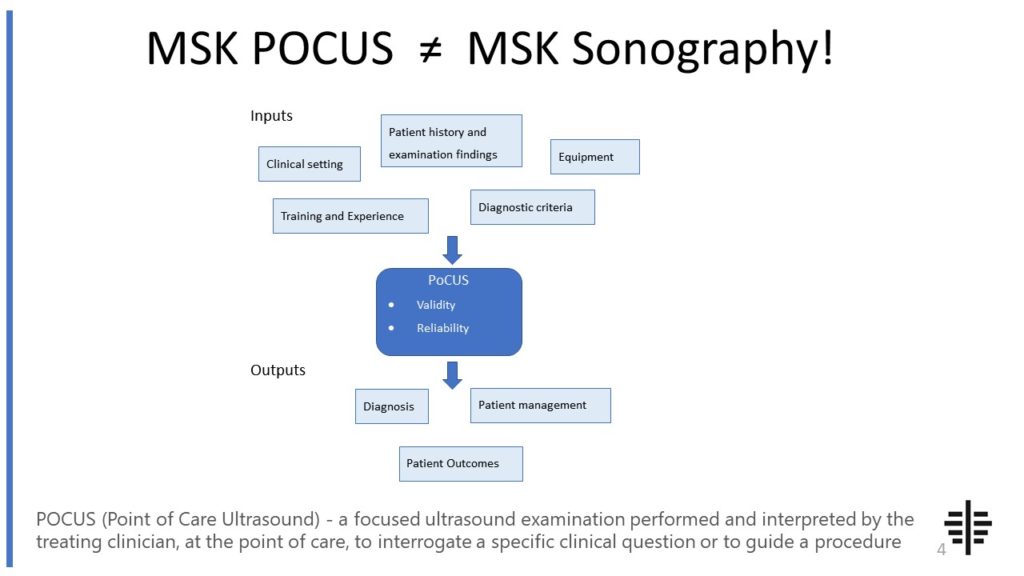
The POCUS process is very different to traditional US based in a radiology establishment. And POCUS practitioners need to be aware of those factors, unique to their particular situation, that influence diagnostic accuracy. That was the topic I presented at the plenary session of the NZAMM Annual Scientific Meeting in Wellington. A picture says 1000 ...
Posted by on 2022-10-04
We’re proud to announce that the New Zealand College of Musculoskeletal Medicine has endorsed our POCUS courses for CME and as part of vocational training. The NZCMM is responsible for setting the high standards and training of Specialist Musculoskeletal Medicine Physicians in New Zealand. NZCMM endorsement is an acknowledgement that our courses meet these standards. ...

Posted by on 2022-06-23
Yes, ultrasound is able to differentiate between partial and complete tendon tears. By visualizing the tendon structure and assessing the continuity of the fibers, ultrasound can determine the extent of the tear. Partial tendon tears involve a disruption of some but not all of the tendon fibers, while complete tendon tears involve a complete rupture of the tendon. Ultrasound can accurately identify the location and extent of the tear, allowing for appropriate treatment planning.

While ultrasound is a valuable tool for tendon tear diagnosis, it does have some limitations and drawbacks. One limitation is that ultrasound is operator-dependent, meaning that the quality of the images and the accuracy of the diagnosis can vary depending on the skill and experience of the ultrasound technician. Additionally, ultrasound may not be able to visualize deep-seated or small tendon tears as effectively as other imaging techniques such as magnetic resonance imaging (MRI). In some cases, further imaging may be necessary to confirm the diagnosis or provide additional information.
Ultrasound-guided treatment for tendon tears has several advantages compared to traditional treatment methods. By using ultrasound to guide the placement of injections or surgical interventions, the accuracy and precision of the treatment can be improved. Ultrasound allows for real-time visualization of the needle or surgical instruments, ensuring that they are accurately placed within the tendon or surrounding tissues. This can lead to better outcomes and reduced risk of complications. Additionally, ultrasound-guided treatment can be performed in an outpatient setting, reducing the need for hospitalization and allowing for faster recovery.

Yes, ultrasound can be used to monitor the healing progress of tendon tears. By regularly performing ultrasound examinations, the healing process of the tendon can be assessed. Ultrasound can visualize changes in the tendon structure, such as the formation of scar tissue or the restoration of normal tendon fibers. This allows for the monitoring of the healing process and can help guide the rehabilitation and treatment plan. Ultrasound can also detect any complications or re-tears that may occur during the healing process, allowing for timely intervention.
There are generally no specific precautions or preparations that need to be taken before undergoing an ultrasound for tendon tear diagnosis. However, it is important to inform the healthcare provider about any allergies or sensitivities to ultrasound gel or latex, as these may be used during the procedure. It is also important to wear loose-fitting clothing that can be easily removed or adjusted to allow access to the area being examined. The healthcare provider may provide specific instructions regarding fasting or medication use prior to the ultrasound, depending on the individual case. It is always best to follow the instructions provided by the healthcare provider to ensure the best possible ultrasound examination.

Musculoskeletal ultrasound plays a crucial role in the diagnosis of muscle tears by providing detailed imaging of the affected area. This non-invasive imaging technique utilizes high-frequency sound waves to create real-time images of the musculoskeletal system, allowing healthcare professionals to visualize the extent and location of the tear. By examining the ultrasound images, medical practitioners can identify specific features associated with muscle tears, such as hypoechoic areas, disruption of muscle fibers, and irregularities in the muscle contour. Additionally, musculoskeletal ultrasound enables the assessment of surrounding structures, such as tendons and ligaments, which can help determine the severity and potential complications of the tear. The use of musculoskeletal ultrasound in diagnosing muscle tears enhances accuracy and aids in the development of appropriate treatment plans for patients.
When using musculoskeletal ultrasound to evaluate pediatric patients, there are several important considerations to keep in mind. Firstly, it is crucial to take into account the unique anatomical and physiological characteristics of pediatric musculoskeletal structures. This includes understanding the growth plates, epiphyses, and apophyses that are still developing in children. Additionally, the sonographer must be skilled in adapting the ultrasound technique to accommodate the smaller size and thinner subcutaneous tissue of pediatric patients. It is also important to consider the potential challenges in obtaining cooperation and maintaining patient stillness during the examination, as children may be more prone to movement and anxiety. Furthermore, the choice of transducer and imaging settings should be carefully selected to optimize image quality while minimizing potential harm to the pediatric patient. Overall, a thorough understanding of pediatric musculoskeletal ultrasound techniques and considerations is essential for accurate and safe evaluation of pediatric patients.
Musculoskeletal ultrasound has the potential to differentiate between benign and malignant lymphadenopathy. This imaging technique utilizes high-frequency sound waves to produce detailed images of the musculoskeletal system, including lymph nodes. By assessing various characteristics such as size, shape, echogenicity, vascularity, and the presence of necrosis or calcifications, musculoskeletal ultrasound can provide valuable information for distinguishing between benign and malignant lymphadenopathy. Additionally, the use of Doppler ultrasound can help evaluate blood flow patterns within the lymph nodes, which can further aid in the differentiation process. However, it is important to note that while musculoskeletal ultrasound can provide valuable insights, a definitive diagnosis of malignancy often requires further evaluation through techniques such as biopsy or fine-needle aspiration.
Musculoskeletal ultrasound has been found to be an effective diagnostic tool for avulsion fractures. Avulsion fractures occur when a tendon or ligament pulls away a small piece of bone. This type of fracture can be difficult to detect using traditional imaging techniques such as X-rays. However, musculoskeletal ultrasound, which uses high-frequency sound waves to create images of the body's soft tissues, has shown promise in accurately diagnosing avulsion fractures. The ultrasound can provide detailed images of the affected area, allowing healthcare professionals to visualize the extent of the fracture and assess the surrounding soft tissues for any additional damage. Additionally, musculoskeletal ultrasound is non-invasive and does not involve exposure to ionizing radiation, making it a safe and preferred option for diagnosing avulsion fractures.
Musculoskeletal ultrasound plays a crucial role in the evaluation of pigmented villonodular synovitis (PVNS) by providing detailed imaging of the affected joint. This imaging technique allows for the visualization of the synovial lining, which is typically thickened and shows hypervascularity in PVNS. The ultrasound can also detect the presence of nodules or villi within the synovium, which are characteristic features of PVNS. Additionally, musculoskeletal ultrasound can assess the extent of joint involvement, identify any associated joint effusion or synovial cysts, and evaluate the surrounding soft tissues for signs of inflammation or tumor invasion. By providing real-time imaging and Doppler assessment, musculoskeletal ultrasound aids in the accurate diagnosis and monitoring of PVNS, guiding treatment decisions and facilitating targeted interventions such as ultrasound-guided synovial biopsy or aspiration.