

Ultrasound therapy is a non-invasive treatment modality that can be beneficial in the management of tendinopathy. It works by using high-frequency sound waves to generate heat and mechanical vibrations in the affected area. This can help to increase blood flow, promote tissue healing, and reduce pain and inflammation. The heat generated by ultrasound therapy can also help to relax muscles and improve flexibility, which can be particularly beneficial in cases of tendinopathy where there is associated muscle tightness or imbalance.
When using ultrasound therapy for the treatment of tendinopathy, specific parameters are typically used to optimize its effectiveness. The frequency of the ultrasound waves is usually set between 1 and 3 MHz, with a lower frequency being used for deeper tissues and a higher frequency for more superficial structures. The intensity of the ultrasound is typically set between 0.5 and 2 W/cm², depending on the individual's tolerance and the specific goals of the treatment. The duration of each ultrasound session can vary, but it is typically around 5 to 10 minutes per treatment area.
Over the last couple of years, we’ve brought you several courses focusing on Ultrasound Guided Injection Techniques. They’ve been extremely popular, and like our other courses, the feedback has been fantastic. One thing we’ve learnt along the way is that to get the most out of learning injection techniques, a solid grounding in MSK Ultrasound ...
Posted by on 2024-02-10
What a year 2023 was! We’ve loved bringing you courses covering US of the upper and lower limb, and US guided injections through the year. The mix of health professionals from all sorts of backgrounds (Doctors, Nurses, Physios, Sonographers to name a few) has been amazing to be part of. We’ve been humbled by your ...
Posted by on 2023-09-17
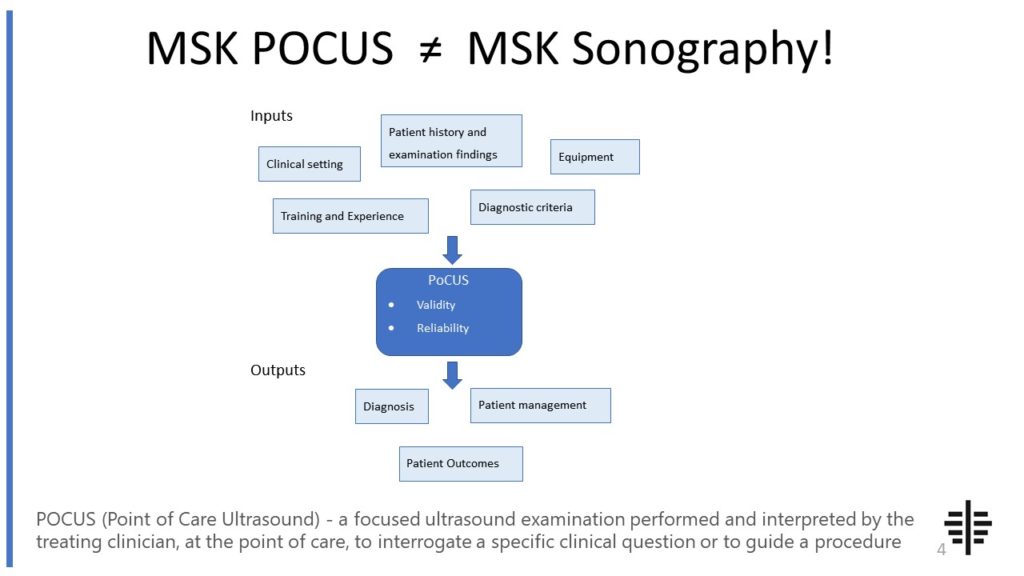
The POCUS process is very different to traditional US based in a radiology establishment. And POCUS practitioners need to be aware of those factors, unique to their particular situation, that influence diagnostic accuracy. That was the topic I presented at the plenary session of the NZAMM Annual Scientific Meeting in Wellington. A picture says 1000 ...
Posted by on 2022-10-04
We’re proud to announce that the New Zealand College of Musculoskeletal Medicine has endorsed our POCUS courses for CME and as part of vocational training. The NZCMM is responsible for setting the high standards and training of Specialist Musculoskeletal Medicine Physicians in New Zealand. NZCMM endorsement is an acknowledgement that our courses meet these standards. ...

Posted by on 2022-06-23
Ultrasound therapy can be used as a standalone treatment for tendinopathy, but it is often combined with other interventions to maximize its benefits. This may include exercises to strengthen and stretch the affected tendon, manual therapy techniques to improve joint mobility and alignment, and other modalities such as ice or heat therapy. The combination of ultrasound therapy with these other interventions can help to address the underlying causes of tendinopathy and provide a more comprehensive approach to treatment.

While ultrasound therapy is generally considered safe, there are some potential side effects and risks associated with its use for tendinopathy. These can include mild discomfort or pain during the treatment, skin irritation or burns if the ultrasound head is not properly applied or if the intensity is too high, and the potential for exacerbation of symptoms if the treatment is not properly tailored to the individual's specific condition. It is important for healthcare professionals to carefully assess each patient and adjust the parameters of the ultrasound therapy accordingly to minimize these risks.
Ultrasound therapy promotes healing and reduces pain in tendinopathy through several mechanisms. The mechanical vibrations generated by the ultrasound waves can help to break down scar tissue and adhesions in the affected tendon, promoting tissue remodeling and regeneration. The heat generated by the ultrasound can increase blood flow to the area, bringing in oxygen and nutrients necessary for tissue repair. Additionally, the increased blood flow can help to remove waste products and inflammatory substances, reducing pain and inflammation in the tendon.

The frequency and duration of ultrasound therapy sessions for tendinopathy can vary depending on the individual's specific condition and response to treatment. In general, it is recommended to have ultrasound therapy sessions 2 to 3 times per week initially, with a gradual reduction in frequency as symptoms improve. Each session typically lasts around 5 to 10 minutes per treatment area, but this can be adjusted based on the individual's tolerance and the specific goals of the treatment. It is important to work with a healthcare professional to determine the most appropriate frequency and duration of ultrasound therapy for each individual.
While ultrasound therapy is generally safe, there are some precautions and contraindications to consider when using it in patients with tendinopathy. It should not be used over areas of infection or open wounds, as it can potentially spread the infection or delay wound healing. Ultrasound therapy should also be used with caution in individuals with certain medical conditions, such as cancer, deep vein thrombosis, or pacemakers, as it may not be appropriate or may require special considerations. It is important for healthcare professionals to thoroughly assess each patient's medical history and condition before using ultrasound therapy for tendinopathy.

Musculoskeletal ultrasound plays a crucial role in the diagnosis of muscle tears by providing detailed imaging of the affected area. This non-invasive imaging technique utilizes high-frequency sound waves to create real-time images of the musculoskeletal system, allowing healthcare professionals to visualize the extent and location of the tear. By examining the ultrasound images, medical practitioners can identify specific features associated with muscle tears, such as hypoechoic areas, disruption of muscle fibers, and irregularities in the muscle contour. Additionally, musculoskeletal ultrasound enables the assessment of surrounding structures, such as tendons and ligaments, which can help determine the severity and potential complications of the tear. The use of musculoskeletal ultrasound in diagnosing muscle tears enhances accuracy and aids in the development of appropriate treatment plans for patients.
When using musculoskeletal ultrasound to evaluate pediatric patients, there are several important considerations to keep in mind. Firstly, it is crucial to take into account the unique anatomical and physiological characteristics of pediatric musculoskeletal structures. This includes understanding the growth plates, epiphyses, and apophyses that are still developing in children. Additionally, the sonographer must be skilled in adapting the ultrasound technique to accommodate the smaller size and thinner subcutaneous tissue of pediatric patients. It is also important to consider the potential challenges in obtaining cooperation and maintaining patient stillness during the examination, as children may be more prone to movement and anxiety. Furthermore, the choice of transducer and imaging settings should be carefully selected to optimize image quality while minimizing potential harm to the pediatric patient. Overall, a thorough understanding of pediatric musculoskeletal ultrasound techniques and considerations is essential for accurate and safe evaluation of pediatric patients.
Musculoskeletal ultrasound has the potential to differentiate between benign and malignant lymphadenopathy. This imaging technique utilizes high-frequency sound waves to produce detailed images of the musculoskeletal system, including lymph nodes. By assessing various characteristics such as size, shape, echogenicity, vascularity, and the presence of necrosis or calcifications, musculoskeletal ultrasound can provide valuable information for distinguishing between benign and malignant lymphadenopathy. Additionally, the use of Doppler ultrasound can help evaluate blood flow patterns within the lymph nodes, which can further aid in the differentiation process. However, it is important to note that while musculoskeletal ultrasound can provide valuable insights, a definitive diagnosis of malignancy often requires further evaluation through techniques such as biopsy or fine-needle aspiration.
Musculoskeletal ultrasound has been found to be an effective diagnostic tool for avulsion fractures. Avulsion fractures occur when a tendon or ligament pulls away a small piece of bone. This type of fracture can be difficult to detect using traditional imaging techniques such as X-rays. However, musculoskeletal ultrasound, which uses high-frequency sound waves to create images of the body's soft tissues, has shown promise in accurately diagnosing avulsion fractures. The ultrasound can provide detailed images of the affected area, allowing healthcare professionals to visualize the extent of the fracture and assess the surrounding soft tissues for any additional damage. Additionally, musculoskeletal ultrasound is non-invasive and does not involve exposure to ionizing radiation, making it a safe and preferred option for diagnosing avulsion fractures.
Musculoskeletal ultrasound plays a crucial role in the evaluation of pigmented villonodular synovitis (PVNS) by providing detailed imaging of the affected joint. This imaging technique allows for the visualization of the synovial lining, which is typically thickened and shows hypervascularity in PVNS. The ultrasound can also detect the presence of nodules or villi within the synovium, which are characteristic features of PVNS. Additionally, musculoskeletal ultrasound can assess the extent of joint involvement, identify any associated joint effusion or synovial cysts, and evaluate the surrounding soft tissues for signs of inflammation or tumor invasion. By providing real-time imaging and Doppler assessment, musculoskeletal ultrasound aids in the accurate diagnosis and monitoring of PVNS, guiding treatment decisions and facilitating targeted interventions such as ultrasound-guided synovial biopsy or aspiration.