

Ultrasound therapy helps in the healing process of muscle tears by promoting tissue repair and reducing inflammation. When ultrasound waves are applied to the affected area, they penetrate deep into the muscle tissue, causing a vibration that increases blood flow and oxygen delivery to the injured area. This increased blood flow helps to remove waste products and deliver essential nutrients to the damaged muscle fibers, aiding in the healing process. Additionally, ultrasound therapy can help to break down scar tissue and improve the flexibility and range of motion in the injured muscle.
There are several specific benefits of using ultrasound for muscle tear treatment compared to other modalities. Firstly, ultrasound therapy is non-invasive, meaning it does not require any surgical procedures or injections. This makes it a safer and more comfortable option for patients. Secondly, ultrasound therapy is highly targeted, allowing for precise treatment of the injured area. This targeted approach helps to minimize damage to surrounding healthy tissues and promotes faster healing. Lastly, ultrasound therapy is a cost-effective treatment option, as it does not require expensive equipment or extensive training to administer.
Over the last couple of years, we’ve brought you several courses focusing on Ultrasound Guided Injection Techniques. They’ve been extremely popular, and like our other courses, the feedback has been fantastic. One thing we’ve learnt along the way is that to get the most out of learning injection techniques, a solid grounding in MSK Ultrasound ...
Posted by on 2024-02-10
What a year 2023 was! We’ve loved bringing you courses covering US of the upper and lower limb, and US guided injections through the year. The mix of health professionals from all sorts of backgrounds (Doctors, Nurses, Physios, Sonographers to name a few) has been amazing to be part of. We’ve been humbled by your ...
Posted by on 2023-09-17
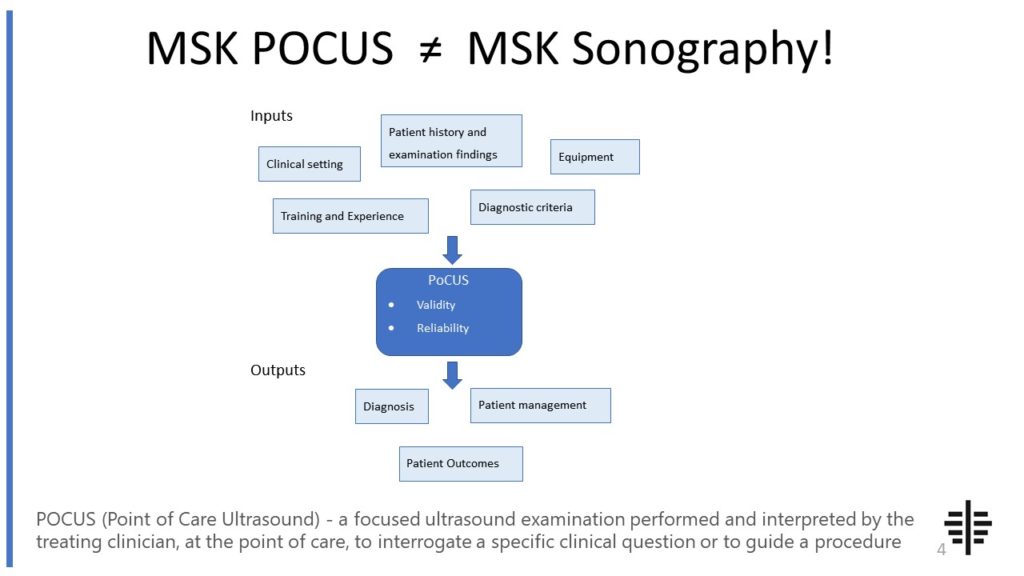
The POCUS process is very different to traditional US based in a radiology establishment. And POCUS practitioners need to be aware of those factors, unique to their particular situation, that influence diagnostic accuracy. That was the topic I presented at the plenary session of the NZAMM Annual Scientific Meeting in Wellington. A picture says 1000 ...
Posted by on 2022-10-04
We’re proud to announce that the New Zealand College of Musculoskeletal Medicine has endorsed our POCUS courses for CME and as part of vocational training. The NZCMM is responsible for setting the high standards and training of Specialist Musculoskeletal Medicine Physicians in New Zealand. NZCMM endorsement is an acknowledgement that our courses meet these standards. ...

Posted by on 2022-06-23
The RNZCUC has endorsed our courses as approved CME. We’re proud to be able to meet the training needs of Urgent Care Physicians, and look forward to meeting you at future courses.

Posted by on 2021-05-30
While ultrasound can provide valuable information about the location and extent of a muscle tear, it is not typically used as a standalone diagnostic tool for determining the severity of a muscle tear. Ultrasound imaging can help visualize the injured muscle and identify any structural abnormalities, such as a partial or complete tear. However, to accurately diagnose the severity of a muscle tear, additional imaging techniques such as MRI or CT scans may be necessary. These imaging modalities provide more detailed information about the extent of the tear and can help guide treatment decisions.

Ultrasound therapy for muscle tears is generally considered safe and well-tolerated. However, there are some potential risks and side effects associated with this treatment. In rare cases, patients may experience mild discomfort or pain during the ultrasound session. Skin irritation or burns can occur if the ultrasound probe is not properly applied or if the treatment duration is too long. It is important for healthcare professionals to follow proper protocols and guidelines to minimize these risks. Additionally, individuals with certain medical conditions, such as deep vein thrombosis or cancer, may not be suitable candidates for ultrasound therapy.
The time it takes for ultrasound therapy to show noticeable improvements in muscle tear healing can vary depending on the severity of the injury and individual factors. In general, patients may start to experience some relief and improvement in symptoms after a few sessions of ultrasound therapy. However, complete healing of a muscle tear can take several weeks to months, and it is important to follow a comprehensive treatment plan that includes rest, physical therapy, and other modalities as recommended by a healthcare professional.

There are specific guidelines and protocols for using ultrasound therapy in the treatment of muscle tears. The treatment duration and frequency may vary depending on the individual case, but typically, ultrasound therapy sessions last between 5 to 10 minutes and are repeated 2 to 3 times per week. The ultrasound probe is applied directly to the skin over the injured muscle, and a conductive gel is used to enhance the transmission of ultrasound waves. The intensity and frequency of the ultrasound waves are adjusted based on the patient's comfort level and the desired therapeutic effect. It is important for healthcare professionals to receive proper training and follow established protocols to ensure safe and effective treatment.
Ultrasound therapy can be used as a standalone treatment for muscle tears, but it is often used in conjunction with other therapies to optimize healing and recovery. In addition to ultrasound therapy, treatment for muscle tears may include rest, ice, compression, and elevation (RICE), physical therapy exercises, pain management techniques, and in some cases, surgical intervention. The combination of these therapies can help to reduce pain, promote tissue repair, restore muscle strength and flexibility, and prevent further injury. The specific treatment approach will depend on the severity of the muscle tear and the individual needs of the patient. It is important for healthcare professionals to develop a comprehensive treatment plan tailored to each patient's unique situation.

Typical ultrasound findings in patients with herniated discs include the visualization of disc protrusion or extrusion, nerve root compression, and spinal canal stenosis. Ultrasound can detect the displacement of the disc material beyond the normal boundaries of the intervertebral space, as well as the compression of adjacent nerve roots. Additionally, ultrasound can identify the narrowing of the spinal canal due to the herniated disc, which can lead to symptoms such as radiculopathy or myelopathy. Other ultrasound findings may include the presence of inflammation, edema, or vascular changes in the surrounding tissues. Overall, ultrasound imaging provides valuable information for the diagnosis and management of herniated discs, allowing for targeted treatment approaches.
Musculoskeletal ultrasound offers several advantages over other imaging modalities when it comes to guiding therapeutic interventions. Firstly, it provides real-time imaging, allowing for dynamic visualization of the musculoskeletal structures during the intervention. This enables the healthcare provider to accurately target the specific area of interest and ensure precise needle placement or delivery of therapeutic agents. Additionally, musculoskeletal ultrasound is a non-invasive and radiation-free imaging technique, making it a safer option for both the patient and the healthcare provider. It also offers excellent soft tissue resolution, allowing for the visualization of tendons, ligaments, muscles, and other soft tissue structures with high detail. This can be particularly beneficial when performing interventions such as injections or aspirations, as it helps to avoid damage to surrounding structures. Furthermore, musculoskeletal ultrasound is a portable and cost-effective imaging modality, making it easily accessible in various clinical settings. Overall, the use of musculoskeletal ultrasound for guiding therapeutic interventions provides real-time visualization, safety, excellent soft tissue resolution, and cost-effectiveness, making it a valuable tool in the field of musculoskeletal medicine.
Musculoskeletal ultrasound plays a crucial role in the diagnosis of Achilles tendonitis by providing detailed imaging of the affected area. This imaging technique utilizes high-frequency sound waves to create real-time images of the musculoskeletal system, allowing healthcare professionals to visualize the Achilles tendon and surrounding structures. By examining the ultrasound images, medical practitioners can identify signs of inflammation, thickening, or degeneration in the tendon, which are characteristic of Achilles tendonitis. Additionally, musculoskeletal ultrasound enables the assessment of blood flow within the tendon, aiding in the differentiation between Achilles tendonitis and other conditions such as Achilles tendon rupture. Overall, the use of musculoskeletal ultrasound in diagnosing Achilles tendonitis enhances accuracy and facilitates appropriate treatment planning for patients.
Musculoskeletal ultrasound plays a crucial role in the diagnosis of osteoarthritis by providing detailed imaging of the affected joints and surrounding tissues. This non-invasive imaging technique utilizes high-frequency sound waves to create real-time images of the musculoskeletal system, allowing healthcare professionals to assess the extent of joint damage and identify characteristic features of osteoarthritis, such as joint space narrowing, osteophyte formation, and synovial thickening. Additionally, musculoskeletal ultrasound enables the visualization of soft tissues, including tendons, ligaments, and muscles, which can help determine the presence of associated injuries or inflammation. By providing a comprehensive assessment of the affected joints, musculoskeletal ultrasound aids in the accurate diagnosis and monitoring of osteoarthritis, facilitating appropriate treatment planning and management strategies.
Musculoskeletal ultrasound findings in patients with fibromyalgia typically show no specific abnormalities or structural damage. However, there may be evidence of increased muscle echogenicity, indicating inflammation or edema in the affected muscles. Additionally, hypervascularity may be observed, suggesting increased blood flow to the affected areas. These findings are consistent with the underlying pathophysiology of fibromyalgia, which involves central sensitization and abnormal pain processing rather than structural abnormalities. It is important to note that musculoskeletal ultrasound is primarily used to rule out other potential causes of musculoskeletal pain and is not a diagnostic tool for fibromyalgia.
Musculoskeletal ultrasound can be a useful tool in the diagnosis of ankylosing spondylitis. This imaging technique allows for the visualization of the musculoskeletal system, including the spine and joints, providing valuable information about the presence of inflammation and structural changes associated with ankylosing spondylitis. By using high-frequency sound waves, musculoskeletal ultrasound can detect signs such as synovitis, enthesitis, and bone erosions, which are characteristic features of ankylosing spondylitis. Additionally, ultrasound can assess the severity and extent of disease involvement, aiding in the monitoring of disease progression and response to treatment. While musculoskeletal ultrasound is not the sole diagnostic tool for ankylosing spondylitis, it can complement other clinical and imaging modalities, such as X-rays and magnetic resonance imaging (MRI), to provide a comprehensive evaluation of the disease.