

Ultrasound is commonly used in the diagnosis of musculoskeletal injuries due to its ability to provide real-time imaging of soft tissues, such as muscles, tendons, and ligaments. It can help identify abnormalities such as tears, strains, or inflammation in these structures. Ultrasound can also be used to assess the surrounding blood vessels and nerves, providing a comprehensive evaluation of the injury. Additionally, ultrasound is non-invasive and does not involve exposure to ionizing radiation, making it a safe and preferred imaging modality for musculoskeletal injuries.
The use of ultrasound for guided injections in orthopedics offers several advantages. Firstly, ultrasound allows for real-time visualization of the needle and the target area, ensuring accurate needle placement and reducing the risk of complications. This is particularly beneficial when injecting into small or deep structures, such as joints or bursae. Secondly, ultrasound can help identify any anatomical variations or abnormalities that may affect the injection procedure. Lastly, ultrasound-guided injections have been shown to improve the accuracy and efficacy of the injection, leading to better patient outcomes and potentially reducing the need for additional interventions.
We’re proud to announce that the New Zealand College of Musculoskeletal Medicine has endorsed our POCUS courses for CME and as part of vocational training. The NZCMM is responsible for setting the high standards and training of Specialist Musculoskeletal Medicine Physicians in New Zealand. NZCMM endorsement is an acknowledgement that our courses meet these standards. ...

Posted by on 2022-06-23
Over the last couple of years, we’ve brought you several courses focusing on Ultrasound Guided Injection Techniques. They’ve been extremely popular, and like our other courses, the feedback has been fantastic. One thing we’ve learnt along the way is that to get the most out of learning injection techniques, a solid grounding in MSK Ultrasound ...
Posted by on 2024-02-10
What a year 2023 was! We’ve loved bringing you courses covering US of the upper and lower limb, and US guided injections through the year. The mix of health professionals from all sorts of backgrounds (Doctors, Nurses, Physios, Sonographers to name a few) has been amazing to be part of. We’ve been humbled by your ...
Posted by on 2023-09-17
The RNZCUC has endorsed our courses as approved CME. We’re proud to be able to meet the training needs of Urgent Care Physicians, and look forward to meeting you at future courses.

Posted by on 2021-05-30
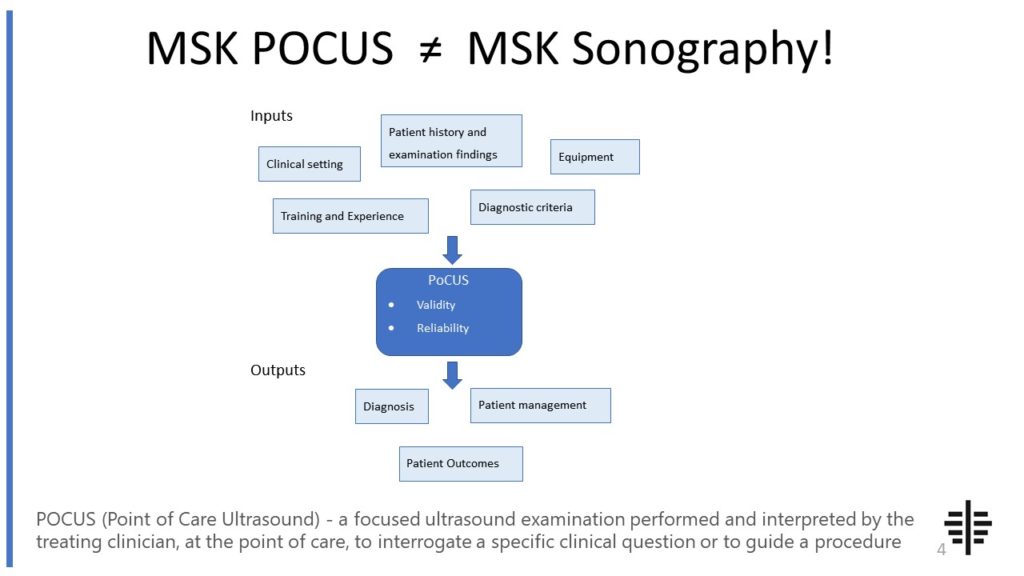
The POCUS process is very different to traditional US based in a radiology establishment. And POCUS practitioners need to be aware of those factors, unique to their particular situation, that influence diagnostic accuracy. That was the topic I presented at the plenary session of the NZAMM Annual Scientific Meeting in Wellington. A picture says 1000 ...
Posted by on 2022-10-04
Ultrasound plays a crucial role in the assessment of tendon and ligament injuries. It can provide detailed imaging of these structures, allowing for the visualization of tears, ruptures, or degenerative changes. Ultrasound can also assess the surrounding tissues, such as muscles and bursae, to determine the extent of the injury and identify any associated abnormalities. Additionally, ultrasound can be used to evaluate the vascularity of tendons and ligaments, which is important for determining the healing potential and guiding treatment decisions. Overall, ultrasound is a valuable tool in the assessment and management of tendon and ligament injuries.

While ultrasound is a useful imaging modality for musculoskeletal injuries, it does have limitations in detecting fractures in orthopedics. Ultrasound is primarily used to visualize soft tissues and is less effective in evaluating bony structures. Fractures may not be clearly visible on ultrasound, especially if they are small or located deep within the body. In these cases, other imaging modalities such as X-ray, CT scan, or MRI may be more appropriate for detecting and assessing fractures. However, ultrasound can still be used to evaluate the surrounding soft tissues and assess for any associated injuries.
Ultrasound is commonly used in the evaluation of joint effusions and synovitis. It can accurately detect the presence of fluid within a joint, which is indicative of an effusion. Ultrasound can also assess the characteristics of the fluid, such as its location, volume, and composition. This information can help determine the underlying cause of the effusion, such as inflammation or infection. Additionally, ultrasound can visualize the synovium, which lines the joint and can become inflamed in conditions such as rheumatoid arthritis. Overall, ultrasound is a valuable tool in the evaluation and management of joint effusions and synovitis.

Yes, ultrasound can be used to assess muscle and nerve injuries in orthopedics. Ultrasound can provide detailed imaging of the muscles, allowing for the visualization of tears, strains, or atrophy. It can also assess the surrounding tissues, such as tendons and fascia, to determine the extent of the injury and identify any associated abnormalities. Additionally, ultrasound can be used to evaluate the nerves, visualizing their course, size, and any signs of compression or injury. This can help in the diagnosis and management of conditions such as nerve entrapment or peripheral neuropathy. Overall, ultrasound is a valuable tool in the assessment of muscle and nerve injuries in orthopedics.
The potential complications or risks associated with ultrasound-guided procedures in orthopedics are generally minimal. Ultrasound is a non-invasive imaging modality that does not involve exposure to ionizing radiation, reducing the risk of radiation-related complications. The procedure itself is typically well-tolerated and does not require sedation or anesthesia. However, there may be some discomfort or pressure during the procedure, particularly if the area being examined is already painful or inflamed. In rare cases, there may be a risk of infection or bleeding at the site of the procedure, but this is generally low. Overall, ultrasound-guided procedures in orthopedics are considered safe and have a low risk of complications.

Pseudogout, also known as calcium pyrophosphate deposition disease (CPPD), is a condition characterized by the deposition of calcium pyrophosphate crystals in the joints. Ultrasound findings in patients with pseudogout typically show hyperechoic or bright white areas within the affected joints, indicating the presence of these crystals. The crystals can be seen as irregular, punctate, or linear hyperechoic structures within the joint space. Additionally, ultrasound may reveal joint effusion, synovial thickening, and cartilage calcification, which are common features of pseudogout. The presence of these ultrasound findings can help in the diagnosis and management of patients with pseudogout, allowing for appropriate treatment and monitoring of the disease.
Chondromalacia patellae is a condition characterized by the softening and degeneration of the cartilage on the underside of the patella, or kneecap. When performing an ultrasound examination on patients with chondromalacia patellae, typical findings may include irregularity or thinning of the articular cartilage, presence of fissures or defects in the cartilage surface, and increased echogenicity or brightness of the cartilage. Additionally, the ultrasound may reveal the presence of joint effusion or fluid accumulation within the knee joint, as well as synovial hypertrophy or thickening of the synovial lining. These ultrasound findings are indicative of the pathological changes occurring in the patellar cartilage and can help in the diagnosis and management of chondromalacia patellae.
Musculoskeletal ultrasound offers several advantages for diagnosing ganglion cysts. Firstly, it provides real-time imaging, allowing for immediate visualization of the cyst and surrounding structures. This enables the clinician to accurately assess the size, location, and extent of the cyst, as well as any associated joint or tendon involvement. Additionally, musculoskeletal ultrasound is non-invasive and does not involve exposure to ionizing radiation, making it a safe and preferred imaging modality, especially for pediatric and pregnant patients. The high-frequency sound waves used in ultrasound also provide excellent resolution, allowing for detailed evaluation of the cyst's internal characteristics, such as its contents and vascularity. This aids in distinguishing ganglion cysts from other soft tissue masses, such as tumors or synovial cysts. Furthermore, musculoskeletal ultrasound can be performed dynamically, allowing for assessment of the cyst's mobility and changes in size with joint movement. This dynamic evaluation is particularly useful in differentiating ganglion cysts from other conditions, such as tendon sheath cysts or joint effusions. Overall, musculoskeletal ultrasound offers a reliable, safe, and comprehensive diagnostic tool for accurately identifying and characterizing ganglion cysts.
Musculoskeletal ultrasound can be a useful tool for diagnosing infections of the musculoskeletal system. This imaging technique utilizes high-frequency sound waves to create detailed images of the muscles, bones, and joints. By examining these images, healthcare professionals can identify signs of infection such as fluid accumulation, abscess formation, or soft tissue swelling. Additionally, musculoskeletal ultrasound can help guide the placement of a needle for aspiration or biopsy, allowing for further analysis of the infected area. The use of musculoskeletal ultrasound in diagnosing infections can provide valuable information for healthcare providers, aiding in the accurate and timely treatment of these conditions.
Assessing acromioclavicular joint pathology using musculoskeletal ultrasound presents several challenges. One of the main challenges is the limited visibility of the joint due to its deep location and the presence of surrounding structures such as the clavicle and acromion. This can make it difficult to obtain clear and accurate images of the joint. Additionally, the acromioclavicular joint is a small and complex joint, which requires a high level of expertise and skill to properly assess using ultrasound. The interpretation of ultrasound images of the acromioclavicular joint also requires a thorough understanding of the anatomy and pathology of the joint, as well as knowledge of the various ultrasound techniques and settings that can optimize image quality. Furthermore, the acromioclavicular joint is prone to a variety of pathologies, including osteoarthritis, ligamentous injuries, and degenerative changes, which can further complicate the assessment process. Overall, while musculoskeletal ultrasound can be a valuable tool for assessing acromioclavicular joint pathology, it requires specialized training and expertise to overcome the challenges associated with its use.