

The manipulation of an ultrasound probe plays a crucial role in the quality of the image produced. The angle, pressure, and movement of the probe can significantly impact the clarity and accuracy of the ultrasound image. Proper manipulation ensures that the probe is in the correct position and orientation to capture the desired structures. If the probe is not manipulated correctly, it may result in suboptimal imaging, such as poor resolution, artifacts, or incomplete visualization of the structures of interest. Therefore, skilled manipulation of the ultrasound probe is essential for obtaining high-quality images for accurate diagnosis and treatment planning.
There are various techniques used to manipulate an ultrasound probe during a procedure. These techniques include adjusting the angle of the probe, applying appropriate pressure, and using specific movements to optimize image acquisition. The angle of the probe can be adjusted to obtain different views and perspectives of the structures being examined. Applying the right amount of pressure ensures proper contact between the probe and the patient's skin, allowing for better transmission of ultrasound waves. Movements such as sliding, rocking, or rotating the probe can help visualize structures from different angles and improve image quality. These techniques are tailored to the specific clinical setting and the anatomical structures being assessed.
Over the last couple of years, we’ve brought you several courses focusing on Ultrasound Guided Injection Techniques. They’ve been extremely popular, and like our other courses, the feedback has been fantastic. One thing we’ve learnt along the way is that to get the most out of learning injection techniques, a solid grounding in MSK Ultrasound ...
Posted by on 2024-02-10
What a year 2023 was! We’ve loved bringing you courses covering US of the upper and lower limb, and US guided injections through the year. The mix of health professionals from all sorts of backgrounds (Doctors, Nurses, Physios, Sonographers to name a few) has been amazing to be part of. We’ve been humbled by your ...
Posted by on 2023-09-17
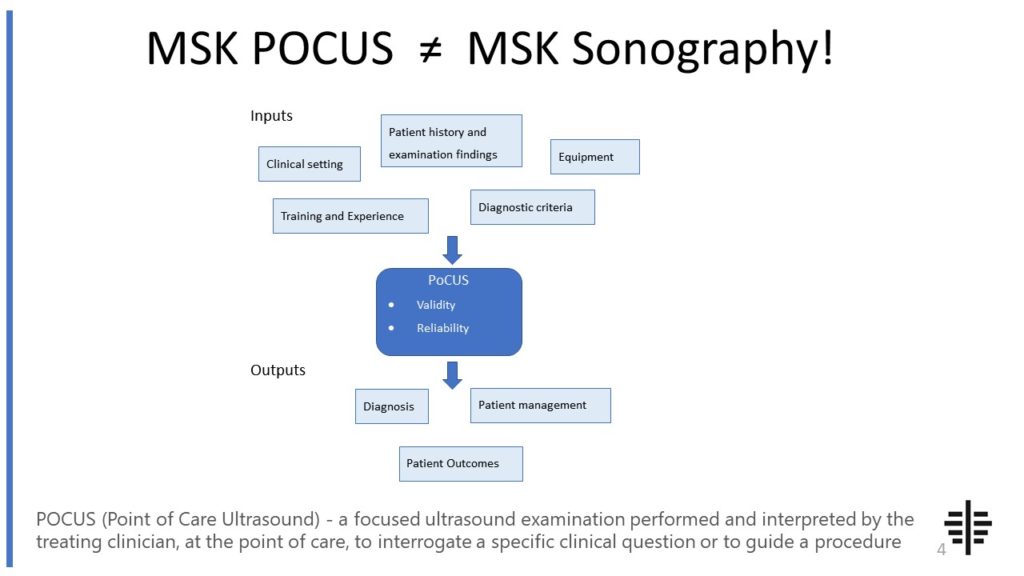
The POCUS process is very different to traditional US based in a radiology establishment. And POCUS practitioners need to be aware of those factors, unique to their particular situation, that influence diagnostic accuracy. That was the topic I presented at the plenary session of the NZAMM Annual Scientific Meeting in Wellington. A picture says 1000 ...
Posted by on 2022-10-04
We’re proud to announce that the New Zealand College of Musculoskeletal Medicine has endorsed our POCUS courses for CME and as part of vocational training. The NZCMM is responsible for setting the high standards and training of Specialist Musculoskeletal Medicine Physicians in New Zealand. NZCMM endorsement is an acknowledgement that our courses meet these standards. ...

Posted by on 2022-06-23
The angle of the ultrasound probe has a significant impact on the visualization of structures. By changing the angle, different planes and perspectives can be obtained, allowing for a comprehensive assessment of the anatomical structures. For example, angling the probe perpendicular to the structure of interest can provide a cross-sectional view, while angling it parallel can offer a longitudinal view. The angle also affects the depth of penetration and the resolution of the image. An optimal angle ensures that the structures are visualized clearly and accurately, while an improper angle may result in distorted or incomplete visualization.

Improper manipulation of an ultrasound probe can lead to potential risks or complications. One of the main risks is the misinterpretation of the ultrasound image, which can result in incorrect diagnosis or treatment decisions. Improper manipulation may also cause discomfort or pain to the patient, especially if excessive pressure is applied. In some cases, it can even lead to injury, such as tissue damage or bruising. Additionally, inadequate manipulation may result in suboptimal image quality, making it challenging to identify and assess the structures of interest accurately. Therefore, proper training and adherence to guidelines for probe manipulation are crucial to minimize these risks and complications.
Yes, the manipulation of an ultrasound probe can be adjusted based on the patient's body habitus or specific anatomical considerations. Different patients may have variations in body size, shape, and tissue characteristics, which can affect the optimal positioning and manipulation of the probe. For example, in patients with a larger body habitus, adjustments may be needed to ensure adequate penetration and visualization of deeper structures. Similarly, specific anatomical considerations, such as the location of organs or the presence of surgical scars, may require modifications in the probe manipulation technique to obtain optimal images. Adapting the manipulation technique to individual patients' needs is essential for obtaining accurate and diagnostically valuable ultrasound images.

There are specific guidelines and recommendations for the manipulation of an ultrasound probe in different clinical settings or procedures. These guidelines are developed by professional organizations and experts in the field of medical imaging. They provide standardized protocols and techniques for probe manipulation to ensure consistent and high-quality imaging. These guidelines may include recommendations on the angle and pressure to be applied, the specific movements to be used, and any patient-specific considerations. Following these guidelines helps to optimize image acquisition, improve diagnostic accuracy, and enhance patient outcomes.
To optimize the manipulation of an ultrasound probe and enhance diagnostic accuracy, several factors should be considered. First, proper training and proficiency in probe manipulation techniques are essential for healthcare professionals performing ultrasound examinations. This ensures that they have the necessary skills to obtain high-quality images. Second, regular calibration and maintenance of the ultrasound equipment are crucial to ensure accurate imaging. Third, effective communication between the sonographer and the interpreting physician is vital to ensure that the desired structures are adequately visualized. Finally, continuous quality improvement initiatives, such as regular audits and feedback, can help identify areas for improvement and enhance the overall quality of ultrasound imaging. By optimizing the manipulation of the ultrasound probe, healthcare providers can improve diagnostic accuracy, facilitate appropriate treatment decisions, and ultimately improve patient outcomes.

Musculoskeletal ultrasound has several limitations when it comes to assessing cartilage integrity. Firstly, the resolution of ultrasound images may not be sufficient to accurately visualize the thin layer of cartilage. This can make it challenging to detect subtle changes or early stages of cartilage damage. Additionally, ultrasound is highly operator-dependent, meaning that the skill and experience of the sonographer can greatly influence the quality and interpretation of the images. Furthermore, ultrasound is limited in its ability to assess the deeper layers of cartilage, as it is primarily used for superficial imaging. This can result in a limited assessment of the overall cartilage integrity. Lastly, ultrasound may not be able to differentiate between different types of cartilage abnormalities, such as degeneration, inflammation, or tears, which can impact the accuracy of the assessment.
Musculoskeletal ultrasound plays a crucial role in the evaluation of joint laxity by providing detailed imaging of the musculoskeletal structures involved. This imaging technique allows for the visualization of ligaments, tendons, and other soft tissues surrounding the joint, enabling the assessment of their integrity and potential laxity. By utilizing high-frequency sound waves, musculoskeletal ultrasound can accurately detect and measure any abnormalities or changes in the joint's stability. Additionally, this imaging modality allows for real-time assessment of joint movement and dynamic evaluation of ligamentous laxity. Overall, musculoskeletal ultrasound provides valuable information for clinicians in diagnosing and monitoring joint laxity, aiding in the development of appropriate treatment plans and interventions.
Musculoskeletal ultrasound is a valuable tool for evaluating hip pathology, but it does come with its challenges. One of the main challenges is the limited field of view that ultrasound provides, which can make it difficult to visualize the entire hip joint and surrounding structures. Additionally, the hip joint is deep within the body, making it challenging to obtain clear and accurate images. The presence of bony structures, such as the femur and pelvis, can also create acoustic shadowing, further hindering the visualization of soft tissues. Furthermore, the hip joint is a complex structure with multiple layers of muscles, tendons, and ligaments, making it challenging to differentiate between normal and abnormal structures. Lastly, operator dependence is another challenge, as the quality of the ultrasound images and the accuracy of the interpretation heavily rely on the skill and experience of the operator.
Musculoskeletal ultrasound offers several advantages over conventional radiography for diagnosing stress fractures. Firstly, ultrasound allows for real-time imaging, providing immediate visualization of the affected area. This enables the clinician to assess the fracture site dynamically, evaluating the extent of the injury and identifying any associated soft tissue damage. Additionally, ultrasound is non-invasive and does not involve exposure to ionizing radiation, making it a safer option, especially for repetitive imaging in athletes or individuals with multiple stress fractures. Furthermore, ultrasound can detect early signs of stress fractures, such as periosteal edema or cortical irregularities, which may not be visible on radiographs. The high resolution and ability to perform dynamic maneuvers, such as stress testing, make ultrasound a valuable tool for accurately diagnosing stress fractures and guiding appropriate treatment decisions.
Typical findings in musculoskeletal ultrasound of patients with calcaneal fractures include the presence of hypoechoic areas within the calcaneus, indicating the presence of bone edema or hematoma. The ultrasound may also reveal disruption or irregularity of the cortical bone, as well as the presence of fracture lines or fragments. In addition, there may be associated soft tissue swelling and inflammation, which can be visualized as increased echogenicity and thickening of the surrounding tissues. Doppler ultrasound may also be used to assess for any associated vascular injury or compromised blood flow. Overall, musculoskeletal ultrasound plays a valuable role in the evaluation and diagnosis of calcaneal fractures, providing detailed imaging of the bony and soft tissue structures involved.
Musculoskeletal ultrasound examinations are commonly performed to evaluate a wide range of conditions and injuries affecting the musculoskeletal system. These examinations are particularly useful in assessing soft tissue structures such as muscles, tendons, ligaments, and bursae. Common indications for performing a musculoskeletal ultrasound examination include the evaluation of acute or chronic pain, swelling, or limited range of motion in a joint or muscle. It can also be used to assess for the presence of fluid collections, such as joint effusions or bursitis. Additionally, musculoskeletal ultrasound can aid in the diagnosis and monitoring of conditions such as tendonitis, tendon tears, muscle strains, ligament injuries, and nerve entrapments. Overall, musculoskeletal ultrasound is a valuable imaging modality that can provide detailed and real-time visualization of the musculoskeletal structures, aiding in the accurate diagnosis and management of various musculoskeletal conditions.