

There are several imaging techniques used to visualize muscles, including magnetic resonance imaging (MRI), ultrasound imaging, computed tomography (CT) scan, X-ray imaging, positron emission tomography (PET) scan, and diffusion tensor imaging (DTI). MRI is a non-invasive technique that uses strong magnetic fields and radio waves to produce detailed images of the muscles. Ultrasound imaging uses high-frequency sound waves to create real-time images of the muscles. CT scan combines X-ray images taken from different angles to create cross-sectional images of the muscles. X-ray imaging uses low-dose radiation to produce images of the bones and soft tissues surrounding the muscles. PET scan involves injecting a radioactive tracer into the body to measure muscle metabolism. DTI is a specialized MRI technique that can provide information about the integrity of muscle fibers.
Magnetic resonance imaging (MRI) is particularly helpful in assessing muscle injuries because it can provide detailed images of the soft tissues, including the muscles. MRI can detect muscle tears, strains, and other types of injuries by visualizing changes in the muscle structure and identifying areas of inflammation or bleeding. It can also help determine the extent and severity of the injury, which is crucial for developing an appropriate treatment plan. Additionally, MRI can be used to monitor the healing process and evaluate the effectiveness of treatment interventions.
Over the last couple of years, we’ve brought you several courses focusing on Ultrasound Guided Injection Techniques. They’ve been extremely popular, and like our other courses, the feedback has been fantastic. One thing we’ve learnt along the way is that to get the most out of learning injection techniques, a solid grounding in MSK Ultrasound ...
Posted by on 2024-02-10
What a year 2023 was! We’ve loved bringing you courses covering US of the upper and lower limb, and US guided injections through the year. The mix of health professionals from all sorts of backgrounds (Doctors, Nurses, Physios, Sonographers to name a few) has been amazing to be part of. We’ve been humbled by your ...
Posted by on 2023-09-17
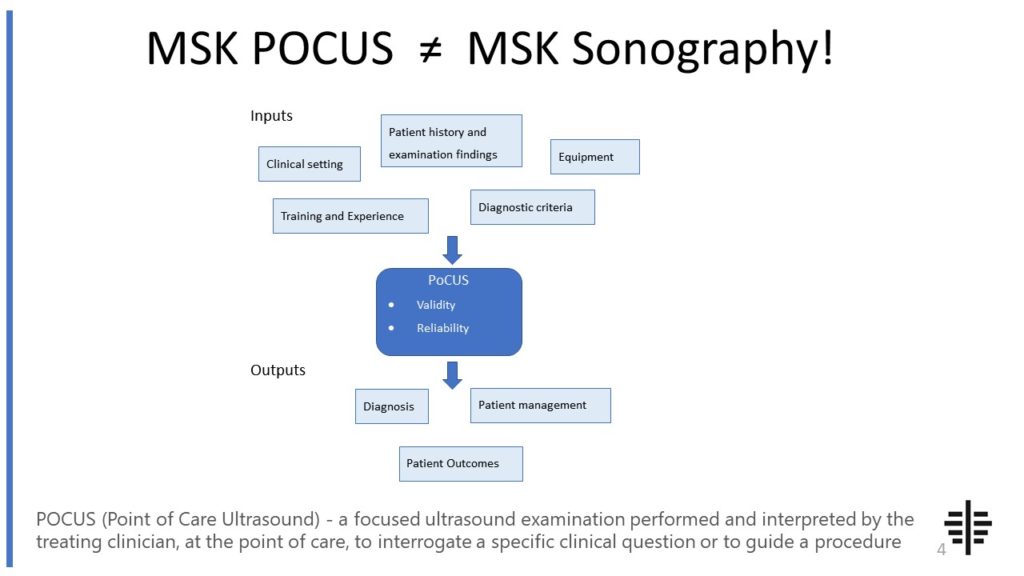
The POCUS process is very different to traditional US based in a radiology establishment. And POCUS practitioners need to be aware of those factors, unique to their particular situation, that influence diagnostic accuracy. That was the topic I presented at the plenary session of the NZAMM Annual Scientific Meeting in Wellington. A picture says 1000 ...
Posted by on 2022-10-04
We’re proud to announce that the New Zealand College of Musculoskeletal Medicine has endorsed our POCUS courses for CME and as part of vocational training. The NZCMM is responsible for setting the high standards and training of Specialist Musculoskeletal Medicine Physicians in New Zealand. NZCMM endorsement is an acknowledgement that our courses meet these standards. ...

Posted by on 2022-06-23
The RNZCUC has endorsed our courses as approved CME. We’re proud to be able to meet the training needs of Urgent Care Physicians, and look forward to meeting you at future courses.

Posted by on 2021-05-30
Ultrasound imaging can be a useful tool for diagnosing muscle tears, but its accuracy depends on the experience and skill of the operator. Ultrasound can provide real-time images of the muscles, allowing for dynamic assessment of muscle function and detecting abnormalities such as tears or ruptures. However, it may not always provide the same level of detail as other imaging techniques like MRI. In some cases, additional imaging modalities may be necessary to confirm the diagnosis or provide more information about the extent of the injury.

Computed tomography (CT) scan offers several advantages for muscle imaging. CT scan can provide detailed cross-sectional images of the muscles, allowing for a more comprehensive assessment of muscle structure and abnormalities. It can also help identify the presence of fractures or other bone-related injuries that may be affecting the muscles. CT scan is particularly useful for evaluating traumatic injuries or complex cases where multiple structures are involved. Additionally, CT scan is a relatively quick imaging technique, making it suitable for emergency situations or patients who cannot tolerate longer imaging procedures.
Positron emission tomography (PET) scan aids in evaluating muscle metabolism by measuring the uptake of a radioactive tracer that is injected into the body. The tracer is typically a form of glucose, which is taken up by metabolically active tissues such as muscles. By detecting the distribution and intensity of the tracer uptake, PET scan can provide information about muscle metabolism and identify areas of increased or decreased activity. This can be helpful in diagnosing muscle disorders, assessing the response to treatment, and monitoring disease progression.

X-ray imaging has several limitations when it comes to muscle assessment. X-rays primarily visualize bones and may not provide sufficient detail of the surrounding soft tissues, including the muscles. While X-rays can help identify fractures or other bone-related injuries that may affect the muscles, they may not be able to detect muscle tears or other soft tissue abnormalities. X-rays also involve exposure to ionizing radiation, which can be a concern, especially in cases where repeated imaging is necessary. Therefore, X-ray imaging is often used in conjunction with other imaging techniques to provide a more comprehensive evaluation of muscle injuries.
Diffusion tensor imaging (DTI) is a specialized MRI technique that provides information about muscle fiber integrity. DTI measures the diffusion of water molecules within the muscle tissue, which can reflect the organization and integrity of muscle fibers. By analyzing the direction and magnitude of water diffusion, DTI can generate maps that visualize the orientation and connectivity of muscle fibers. This information can be valuable for assessing muscle damage, such as fiber disruption or loss, and for understanding the underlying mechanisms of muscle disorders. DTI can also help track changes in muscle fiber integrity over time, providing insights into disease progression or treatment response.

Musculoskeletal ultrasound can be a useful tool in the diagnosis of ankylosing spondylitis. This imaging technique allows for the visualization of the musculoskeletal system, including the spine and joints, providing valuable information about the presence of inflammation and structural changes associated with ankylosing spondylitis. By using high-frequency sound waves, musculoskeletal ultrasound can detect signs such as synovitis, enthesitis, and bone erosions, which are characteristic features of ankylosing spondylitis. Additionally, ultrasound can assess the severity and extent of disease involvement, aiding in the monitoring of disease progression and response to treatment. While musculoskeletal ultrasound is not the sole diagnostic tool for ankylosing spondylitis, it can complement other clinical and imaging modalities, such as X-rays and magnetic resonance imaging (MRI), to provide a comprehensive evaluation of the disease.
Musculoskeletal ultrasound plays a crucial role in the diagnosis of muscle tears by providing detailed imaging of the affected area. This non-invasive imaging technique utilizes high-frequency sound waves to create real-time images of the musculoskeletal system, allowing healthcare professionals to visualize the extent and location of the tear. By examining the ultrasound images, medical practitioners can identify specific features associated with muscle tears, such as hypoechoic areas, disruption of muscle fibers, and irregularities in the muscle contour. Additionally, musculoskeletal ultrasound enables the assessment of surrounding structures, such as tendons and ligaments, which can help determine the severity and potential complications of the tear. The use of musculoskeletal ultrasound in diagnosing muscle tears enhances accuracy and aids in the development of appropriate treatment plans for patients.
When using musculoskeletal ultrasound to evaluate pediatric patients, there are several important considerations to keep in mind. Firstly, it is crucial to take into account the unique anatomical and physiological characteristics of pediatric musculoskeletal structures. This includes understanding the growth plates, epiphyses, and apophyses that are still developing in children. Additionally, the sonographer must be skilled in adapting the ultrasound technique to accommodate the smaller size and thinner subcutaneous tissue of pediatric patients. It is also important to consider the potential challenges in obtaining cooperation and maintaining patient stillness during the examination, as children may be more prone to movement and anxiety. Furthermore, the choice of transducer and imaging settings should be carefully selected to optimize image quality while minimizing potential harm to the pediatric patient. Overall, a thorough understanding of pediatric musculoskeletal ultrasound techniques and considerations is essential for accurate and safe evaluation of pediatric patients.
Musculoskeletal ultrasound has the potential to differentiate between benign and malignant lymphadenopathy. This imaging technique utilizes high-frequency sound waves to produce detailed images of the musculoskeletal system, including lymph nodes. By assessing various characteristics such as size, shape, echogenicity, vascularity, and the presence of necrosis or calcifications, musculoskeletal ultrasound can provide valuable information for distinguishing between benign and malignant lymphadenopathy. Additionally, the use of Doppler ultrasound can help evaluate blood flow patterns within the lymph nodes, which can further aid in the differentiation process. However, it is important to note that while musculoskeletal ultrasound can provide valuable insights, a definitive diagnosis of malignancy often requires further evaluation through techniques such as biopsy or fine-needle aspiration.
Musculoskeletal ultrasound has been found to be an effective diagnostic tool for avulsion fractures. Avulsion fractures occur when a tendon or ligament pulls away a small piece of bone. This type of fracture can be difficult to detect using traditional imaging techniques such as X-rays. However, musculoskeletal ultrasound, which uses high-frequency sound waves to create images of the body's soft tissues, has shown promise in accurately diagnosing avulsion fractures. The ultrasound can provide detailed images of the affected area, allowing healthcare professionals to visualize the extent of the fracture and assess the surrounding soft tissues for any additional damage. Additionally, musculoskeletal ultrasound is non-invasive and does not involve exposure to ionizing radiation, making it a safe and preferred option for diagnosing avulsion fractures.
Musculoskeletal ultrasound plays a crucial role in the evaluation of pigmented villonodular synovitis (PVNS) by providing detailed imaging of the affected joint. This imaging technique allows for the visualization of the synovial lining, which is typically thickened and shows hypervascularity in PVNS. The ultrasound can also detect the presence of nodules or villi within the synovium, which are characteristic features of PVNS. Additionally, musculoskeletal ultrasound can assess the extent of joint involvement, identify any associated joint effusion or synovial cysts, and evaluate the surrounding soft tissues for signs of inflammation or tumor invasion. By providing real-time imaging and Doppler assessment, musculoskeletal ultrasound aids in the accurate diagnosis and monitoring of PVNS, guiding treatment decisions and facilitating targeted interventions such as ultrasound-guided synovial biopsy or aspiration.