

Ultrasound is a valuable tool in diagnosing joint effusion because it allows for real-time visualization of the joint space and surrounding structures. By using high-frequency sound waves, ultrasound can produce detailed images of the joint, including the presence of fluid accumulation. This is particularly useful in diagnosing joint effusion, as it allows for the identification of even small amounts of fluid that may not be easily detected through physical examination alone. Ultrasound can also help determine the location and extent of the effusion, aiding in the diagnosis and treatment planning process.
Specific ultrasound findings that indicate the presence of joint effusion include the visualization of anechoic or hypoechoic fluid within the joint space. Anechoic fluid appears black on the ultrasound image, while hypoechoic fluid appears darker than the surrounding tissues. The presence of fluid can cause distension of the joint capsule, leading to a loss of the normal concave contour of the joint. In addition, ultrasound may reveal synovial thickening or hypertrophy, which can further support the diagnosis of joint effusion.
Over the last couple of years, we’ve brought you several courses focusing on Ultrasound Guided Injection Techniques. They’ve been extremely popular, and like our other courses, the feedback has been fantastic. One thing we’ve learnt along the way is that to get the most out of learning injection techniques, a solid grounding in MSK Ultrasound ...
Posted by on 2024-02-10
What a year 2023 was! We’ve loved bringing you courses covering US of the upper and lower limb, and US guided injections through the year. The mix of health professionals from all sorts of backgrounds (Doctors, Nurses, Physios, Sonographers to name a few) has been amazing to be part of. We’ve been humbled by your ...
Posted by on 2023-09-17
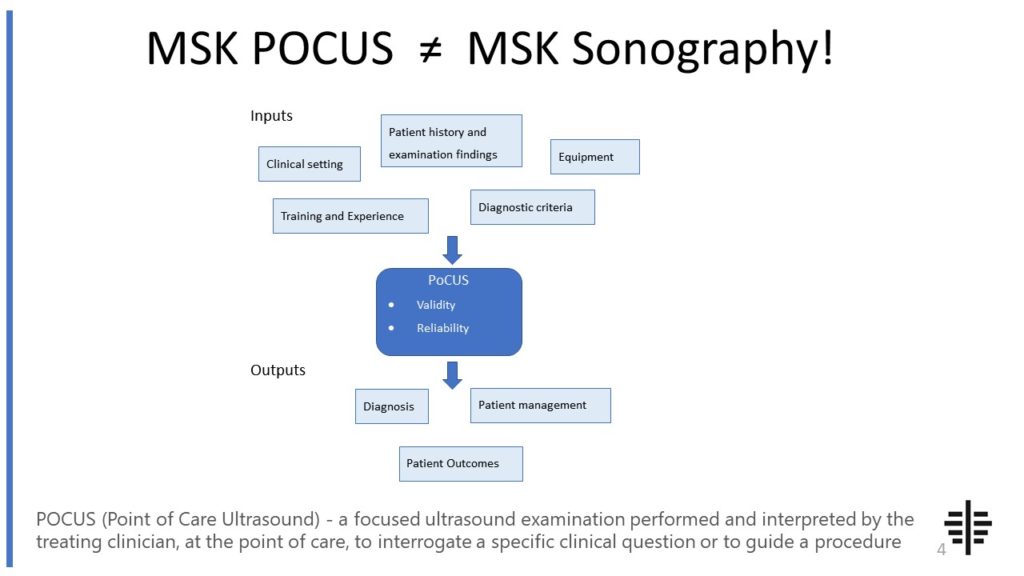
The POCUS process is very different to traditional US based in a radiology establishment. And POCUS practitioners need to be aware of those factors, unique to their particular situation, that influence diagnostic accuracy. That was the topic I presented at the plenary session of the NZAMM Annual Scientific Meeting in Wellington. A picture says 1000 ...
Posted by on 2022-10-04
We’re proud to announce that the New Zealand College of Musculoskeletal Medicine has endorsed our POCUS courses for CME and as part of vocational training. The NZCMM is responsible for setting the high standards and training of Specialist Musculoskeletal Medicine Physicians in New Zealand. NZCMM endorsement is an acknowledgement that our courses meet these standards. ...

Posted by on 2022-06-23
While ultrasound can provide valuable information about the presence and extent of joint effusion, it may not be able to differentiate between different types of effusion, such as inflammatory or non-inflammatory. Additional diagnostic tests, such as laboratory analysis of the synovial fluid, may be necessary to determine the underlying cause of the effusion. However, ultrasound can still play a crucial role in guiding the aspiration of the joint fluid for further analysis, regardless of the type of effusion.

Despite its many advantages, ultrasound does have limitations in detecting joint effusion. One limitation is the operator-dependent nature of the examination. The quality of the ultrasound images and the ability to accurately identify and measure the effusion can vary depending on the skill and experience of the operator. Additionally, certain factors, such as obesity or the presence of gas or bone in the path of the ultrasound beam, can limit the visualization of the joint and the detection of effusion. In these cases, alternative imaging modalities may be necessary.
Ultrasound-guided aspiration of joint effusion improves accuracy and safety by providing real-time visualization of the needle placement and the surrounding structures. This allows for precise targeting of the effusion and minimizes the risk of damaging nearby structures, such as blood vessels or nerves. Ultrasound guidance also increases the success rate of the aspiration procedure, as it helps ensure that an adequate amount of fluid is obtained for analysis. Overall, ultrasound-guided aspiration improves the diagnostic accuracy and reduces the potential complications associated with the procedure.

Alternative imaging modalities that can be used to diagnose joint effusion include magnetic resonance imaging (MRI) and computed tomography (CT). MRI is particularly useful in evaluating soft tissues and can provide detailed information about the extent of the effusion, as well as any associated abnormalities, such as synovial thickening or cartilage damage. CT, on the other hand, is more commonly used in cases where there is suspicion of a fracture or bony abnormality contributing to the joint effusion. Both MRI and CT have their own advantages and limitations, and the choice of imaging modality depends on the specific clinical scenario and available resources.
Yes, ultrasound can be used to monitor the progression or resolution of joint effusion over time. By performing serial ultrasound examinations, healthcare providers can assess changes in the size and characteristics of the effusion, as well as the response to treatment. This can be particularly useful in cases where the underlying cause of the effusion is unclear or when monitoring the effectiveness of therapeutic interventions. Ultrasound allows for repeated non-invasive assessments, reducing the need for more invasive procedures, such as repeated joint aspirations. However, it is important to note that ultrasound findings should always be interpreted in conjunction with the patient's clinical presentation and other diagnostic tests for a comprehensive evaluation.

Musculoskeletal ultrasound plays a crucial role in diagnosing tenosynovitis by providing detailed imaging of the affected tendons and surrounding structures. This imaging technique utilizes high-frequency sound waves to create real-time images of the musculoskeletal system, allowing for the visualization of tendon sheaths and the detection of any abnormalities. By examining the affected area, musculoskeletal ultrasound can identify signs of inflammation, such as thickening of the tendon sheath or the presence of fluid accumulation. Additionally, this imaging modality enables the assessment of tendon integrity, as it can detect tendon tears or degenerative changes. Overall, musculoskeletal ultrasound offers a non-invasive and efficient method for diagnosing tenosynovitis, aiding in the accurate assessment and management of this condition.
Musculoskeletal ultrasound plays a crucial role in diagnosing nerve entrapment syndromes by providing detailed imaging of the musculoskeletal structures and identifying any abnormalities or compressions that may be causing the nerve entrapment. This non-invasive imaging technique allows for real-time visualization of the nerves, surrounding soft tissues, and bony structures, enabling the detection of nerve compression, inflammation, or other pathologies. By using high-frequency sound waves, musculoskeletal ultrasound can accurately assess the nerve's size, shape, and integrity, as well as identify any structural changes or abnormalities in the surrounding tissues. Additionally, musculoskeletal ultrasound can be used to guide diagnostic and therapeutic interventions, such as nerve blocks or injections, providing precise localization of the affected nerve and improving the accuracy of treatment. Overall, musculoskeletal ultrasound is a valuable tool in the diagnosis and management of nerve entrapment syndromes, allowing for early detection and appropriate intervention.
Diagnostic musculoskeletal ultrasound is a non-invasive imaging technique that uses high-frequency sound waves to produce real-time images of the musculoskeletal system. Unlike other imaging techniques such as X-rays, CT scans, and MRI scans, which use ionizing radiation or magnetic fields, ultrasound does not expose the patient to harmful radiation. Additionally, ultrasound is portable and can be performed at the point of care, making it a convenient option for diagnosing musculoskeletal conditions in various settings, including sports medicine clinics and emergency departments. Furthermore, ultrasound allows for dynamic imaging, meaning that the structures being examined can be visualized in motion, providing valuable information about their function and integrity. This is particularly useful in assessing joint stability, tendon and ligament injuries, and muscle tears. Moreover, ultrasound is cost-effective compared to other imaging techniques, making it a preferred choice for initial evaluation and follow-up of musculoskeletal conditions. Overall, diagnostic musculoskeletal ultrasound offers several advantages over other imaging techniques, including its non-invasive nature, portability, real-time imaging capabilities, and cost-effectiveness.
Musculoskeletal ultrasound plays a crucial role in diagnosing plantar fasciitis by providing detailed imaging of the affected area. This non-invasive imaging technique allows healthcare professionals to visualize the plantar fascia, a thick band of tissue located on the bottom of the foot, and assess its condition. Ultrasound can detect abnormalities such as thickening, inflammation, or tears in the plantar fascia, which are indicative of plantar fasciitis. Additionally, musculoskeletal ultrasound can help differentiate plantar fasciitis from other conditions that may present with similar symptoms, such as heel spurs or Achilles tendonitis. By utilizing musculoskeletal ultrasound, healthcare providers can accurately diagnose plantar fasciitis and develop an appropriate treatment plan tailored to the individual patient's needs.
Musculoskeletal ultrasound plays a crucial role in diagnosing stress fractures in the foot by providing detailed imaging of the affected area. This non-invasive imaging technique utilizes high-frequency sound waves to create real-time images of the musculoskeletal structures, including bones, tendons, and ligaments. By using musculoskeletal ultrasound, healthcare professionals can visualize the specific location and extent of the stress fracture, allowing for accurate diagnosis and appropriate treatment planning. Additionally, this imaging modality can help differentiate stress fractures from other foot conditions, such as tendonitis or ligament sprains, by assessing the integrity of the surrounding soft tissues. The ability to visualize the fracture site in real-time and from multiple angles enhances the diagnostic accuracy and aids in monitoring the healing progress of the stress fracture. Overall, musculoskeletal ultrasound is a valuable tool in the diagnosis and management of stress fractures in the foot, providing clinicians with detailed and reliable information for optimal patient care.